
Birth control options
If you’ve been using the same birth control for years, methods are now available for women that you may not even know about (of course, for men, there are basically still two choices: condoms and vasectomy). And one of them might be right for you, depending on what stage of your life you’re at: no desire for kids yet; don’t plan to have any children; still in baby-making mode; or finished having kids.
“Even for doctors, it’s hard to keep up with all of the new developments,” says Dr. Susan Biali of Vancouver. “Plus, both doctors and patients tend to stick with what we’re comfortable with.” Women over 40 may be even less inclined to explore new options because they think that they’re not fertile, according to Dr. Dara Maker, co-medical director at the Bay Centre for Birth Control at Women’s College Hospital in Toronto. “But they can be the most susceptible to unwanted pregnancies because their periods are changing and they don’t have a sense of when they’re most fertile.” Here are some of the options to consider:
Image: iStockphoto.com
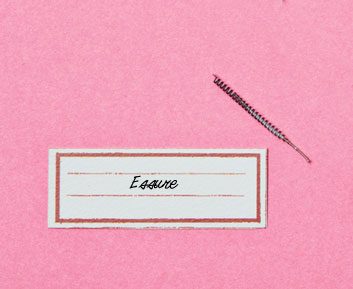
Essure permanent birth control
This non-surgical method of sterilization is low profile yet has been available in Canada since 2002. It’s an alternative to tubal ligation (a.k.a. “having your tubes tied”) and involves blocking the Fallopian tubes. While a tubal ligation requires a general anesthetic, surgery and a two- to three-day recovery, the insertion of an Essure device is an outpatient procedure done with minimal sedation. It’s even more effective for preventing pregnancy (0.17 percent five-year failure rate, compared to one to two percent for tubal ligation).
What’s involved: A gynecologist trained in the procedure places a tiny camera into the vagina and uterus to position a soft flexible nickel and polyester insert into each Fallopian tube. Anesthesia is not required but oral pain relief may be offered beforehand. The procedure takes five minutes and patients are back to their normal activities the next day. “We usually tell people to go home that day. Some women experience a bit of cramping afterwards,” says Dr. John Thiel, clinical professor of obstetrics and gynecology at the University of Saskatchewan and the pioneer of Essure in Canada. Women will continue to get their period afterwards and must use a backup method of birth control for three months until an ultrasound confirms the procedure was successful.
How it works: The polyester is surrounded by a metal coil; while the coil holds it in place, the poly-ester core causes the body to grow a scar that blocks the Fallopian tube and forms a natural barrier, keeping sperm from reaching the egg.
Who it’s best for: Women who are finished having kids, or who are positive they never want them.
When to avoid it: “It’s not reversible, so we really want to make sure women who choose this option are done having kids,” says Thiel.
Where it’s available: Everywhere in Canada except P.E.I., where there aren’t any doctors trained in the procedure. “Uptake has been slow,” says Thiel, “but it’s starting to gain some traction.” The cost of about $1,000 is covered by public health care in some provinces. Check with your doctor.
Image: Tracy Shumate
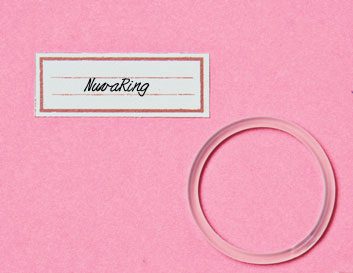
NuvaRing
Approved in Canada about seven years ago, this flexible rubber ring, about two inches in diameter, is a hormonal method of contraception that provides certain advantages over the birth control pill-for example, you don’t need to remember to take it daily, and there’s less breakthrough bleeding. “It’s a fantastic birth control device, but people forget about it, and there is a bit of a ‘yuck’ factor,” says Maker. “Some women don’t feel comfortable inserting it.”
What’s involved: You squeeze the sides together and insert it into the vagina once a month, and leave it in place for three weeks. Then you remove it for the fourth week of the cycle, during menstruation. On Day 1 of a new cycle, you insert a new one.
How it works: The NuvaRing releases a continuous low dose of the hormones estrogen and progestin-comparable to the amount in a low-dose birth control pill-which are absorbed through the vagina. Neither you nor your partner will feel it during intercourse, although it can fall out during sex or from straining during a bowel movement. With perfect use, it’s up to 99 percent effective.
Who it’s best for: Women who often forget to take the pill. It also decreases menstrual flow and cramps, improves acne and reduces PMS symptoms, says Maker. Women who get menstrual migraines sometimes find that the condition improves because the NuvaRing releases hormones at a steady rate.
When to avoid it: Women with a history of heart disease or blood clots, smokers over 35 and women who get migraine with aura are not good candidates.
Where it’s available: By prescription across Canada. It costs about $20 per ring.
Image: Tracy Shumate

Seasonale
Approved in Canada in 2007, this pill alters the menstrual cycle so you menstruate once every three months. (A contraceptive pill called Lybrel that eliminated menstruation for one year came out in the U.S. in 2007 but there were some safety concerns, says Maker, and it never got Health Canada approval.) Reducing your frequency of periods probably sounds pretty great, but it is controversial. “Some people get upset that these products mess with the menstrual cycle, which is an integral part of our bodies,” says Biali. For a lot of women, however, such as those with anemia or menstrual migraine, having fewer periods is quite beneficial, says Maker.
What’s involved: With Seasonale, you take active pills continuously for three months (84 days), followed by seven days of inactive pills, during which time you have your period. Then you start the cycle again. Some women already do essentially the same thing with regular birth control pills if they want to skip their period, say for a vacation or honeymoon, says Biali.
How it works: Seasonale contains a combination of estrogen and progestin, which inhibits ovulation and changes cervical mucus, making it harder for sperm to penetrate the egg. According to the manufacturer, it is 99 percent effective with perfect use.
Who it’s best for: “If you’re having extremely heavy periods, or have anemia, it may be an option, but you still need to address the cause of those problems,” says Biali.
When to avoid it: If you can’t take hormonal methods of birth control, are a smoker over 35 or have a risk of blood clots or heart disease, you should avoid it. It may not be a doctor’s first choice for younger women, either. “When we start women on the pill, it’s usually on the one with the lowest-dose estrogen since they may be on it for years,” says Maker. “Seasonale is fairly low-dose but not super low-dose.”
Where it’s available: By prescription across Canada. It’s a little more expensive than monthly pills: about $50 for a three-month supply.
Image: iStockphoto.com
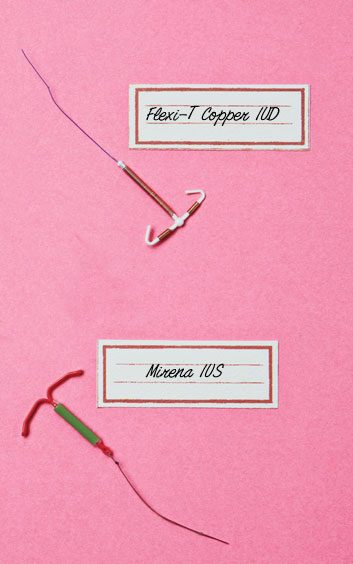
IUD (intrauterine device) and IUS (intrauterine system)
Despite a questionable reputation-thanks to the Dalkon Shield’s faulty design in the 1970s, which increased the risk of pelvic infections-the IUD is regaining popularity. New models, such as the Nova-T and Flexi-T copper IUDs and the Mirena IUS (the only IUS in Canada), are better designed without the same problems. “They’re certainly becoming more popular, with usage up from one percent of Canadian women to five percent in the past decade,” says Maker. “And a lot of it has to do with Mirena, which is really safe-it doesn’t increase rates of infection and is as effective as tubal ligation.”
What’s involved: An obstetrician/gynecologist or family doctor inserts the small T-shaped copper IUD, or the flexible plastic IUS, through the cervix into the uterus. The procedure does not require anesthesia and takes about 15 minutes. “There may be a bitof pain or discomfort, which is treated with pain medication,” says Maker. You’ll be able to feel the threads of an IUD or IUS, which hang from the cervix into the vagina-that tells you it’s in place. If your partner can feel the threads during sex, though, you can ask your doctor to shorten them.
How they work: In the IUD, the copper creates a toxic environment in the uterus that kills sperm. A bit of the hormone progestin is released by the Mirena IUS into the uterus, which thins out the uterine lining and prevents implantation. The IUS is 99 percent and the IUD is 98 percent effective for preventing pregnancy, and both remain in the uterus for five years.
Who they’re best for: The IUD and IUS are marketed to women who have had children (including breastfeeding moms); the devices are easier to insert in women who have had a vaginal birth. But women who’ve never had children can also use them. They can be removed at any time.
When to avoid them: Copper IUDs may make periods heavier with more cramping. According to Maker, the Mirena IUS may actually reduce the amount of menstrual bleeding; some women stop their periods altogether when using it. And the progestin in Mirena means that there’s potential for worsening migraines, but it’s low risk. Women with multiple partners who are at higher risk for pelvic infections (such as chlamydia and gonorrhea) should not use Mirena.
Where they’re available: Across Canada by prescription. The copper IUD costs $70-$150 and Mirena is about $400. Since they work for five years, they may be more cost-effective than condoms or pills in the long run.
Image: Tracy Shumate
Related:
• 6 things you should know about IUDs
• Is it safe to stop your period?
• The truth about adult acne
