
Understanding Alzheimer’s disease risk and sleep
Alzheimer’s disease is a progressive neurological condition that affects over 747,000 Canadians, according to the Alzheimer’s Association. And worldwide, approximately 44 million people are living with dementia, which is why researchers are working overtime to find out more about this disease—and sleep looks like it could be key.
Catching Alzheimer’s disease early
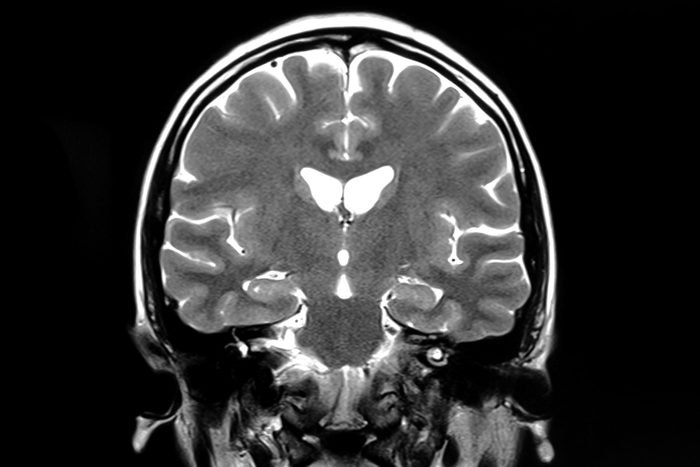
The brain changes caused by Alzheimer’s start slowly and silently—often up to two decades before symptoms like memory loss and confusion appear. In the brain, substances in the brain known as amyloid beta proteins and tau begin to collect into plaques and tangles; as the disease progresses, key areas of the brain can shrink. Here’s where sleep comes in: Some research suggests poor sleep can accelerate Alzheimer’s.

You pull all-nighters
Being groggy the following day isn’t the only reason to avoid going all night: In a study published by Science Magazine, eight volunteers got a good night’s rest and then stayed awake for a full 36 hours. After only one completely sleepless night, participants showed a 51.5 percent increase in the brain protein called tau—which has been linked to Alzheimer’s. In this study, the new tau tangles cropped up in parts of the brain associated with memory—just as they do in people with Alzheimer’s. And in a companion experiment, the researchers found that sleep-deprived mice had twice the amount of tau as well-rested mice.
Find out why females are more likely to get Alzheimer’s than males.

You’re not dealing with your sleep apnea
Does your bed-partner constantly complain about your snoring? If so, it could mean you have sleep apnea, a serious disorder in which people actually stop breathing intermittently throughout the night. A study presented at the 2019 annual meeting of the American Academy of Neurology suggests that people with sleep apnea may have more tau in an area of the brain that aids memory. Of 288 people age 65 and older, those with sleep apnea had 4.5 percent higher levels of tau in their brains compared to people who didn’t have sleep apnea. (
“With sleep apnea, your brain isn’t getting enough oxygen at night, and that increases the risk of cognitive impairment and possibly Alzheimer’s disease,” says Howard Fillit, MD, founding Executive Director and Chief Science Officer of the Alzheimer’s Drug Discovery Foundation. If you notice any of the following less obvious sleep apnea symptoms, talk to your doctor about a sleep evaluation.

You depend on Rx sleeping aids
So, if you’re sleeping poorly, you should see a doctor for a prescription sleeping aid, right? Actually, some sleep drugs may do more harm than good when it comes to Alzheimer’s disease, warns Yuko Hara, PhD, a director with the Alzheimer’s Drug Discovery Foundation. “Long term use of benzodiazepines as sleeping aids may increase the risk for developing Alzheimer’s disease,” she warns.
Some sleep medications are a double-edged sword for people who already show signs of Alzheimer’s, Dr. Fillit says. “As the disease progresses, people with Alzheimer’s disease can develop serious sleep issues, but the use of sedatives can be risky because they can increase the risk of falls and confusion.”
You’re not getting deep, restorative sleep
If you get less slow-wave sleep—the deep sleep you need to consolidate memories and wake up feeling refreshed—you may have higher levels of the brain protein tau, according to a study published in Science Translational Medicine. The study authors point out that being unable to reach deep sleep could either raise Alzheimer’s risk or be an early sign of the disease.

You sleep on your back
Sleeping on your side, rather than on your back or stomach, may be the best position for a healthy brain, finds a recent study. Researchers used MRI scans to monitor the brain’s glymphatic pathway—the system that removes harmful buildup and chemicals from the brain—and how effectively it performed in various sleep positions in mice. It turns out that the brains of mice who slept on their side were more efficient at clearing the kind of waste that can lead to the build-up of beta-amyloid plaque.
The brain cleans itself of Alzheimer’s-related proteins during sleep, explains Michael J. Breus, PhD, a Los Angeles sleep expert and author of several books on sleep including Good Night: The Sleep Doctor’s 4-Week Program to Better Sleep and Better Health. “When you sleep, scientists now think, your glymphatic system steps up its activity to remove potentially harmful debris that has collected over your waking day,” he says. “If you sleep poorly or go without sufficient sleep on a regular basis, you risk missing out on the full effects of this cleansing process.”

You love naps
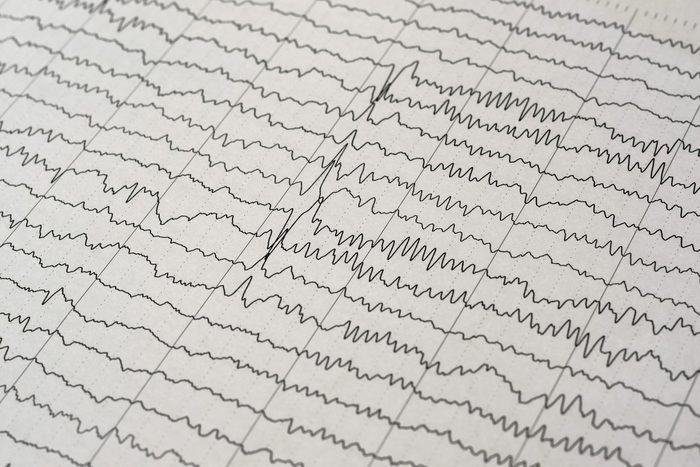
If you make up for poor sleep at night by regularly sneaking catnaps during the day, you may be at an increased risk for Alzheimer’s. A disrupted sleep-wake cycle at night can disrupt your body’s internal clock—circadian rhythm. Breus points to research tracking the sleep patterns of older adults: People with pre-clinical signs of Alzheimer’s all had disrupted sleep-wake cycles, he says. There’s a chicken/egg situation here, says Dr. Breus: Poor sleep could lead to Alzheimer’s, or it could be a symptom of the condition. Plus, these innocent habits could also be ruining your sleep.

Your smartphone obsession
You really meant to hit the hay early, but instead, you’re engrossed in Instagram stories and responding to texts. Using your phone at night can disrupt your circadian rhythms, which researchers have linked to an increased risk for Alzheimer’s, Dr. Fillit says. Reset your circadian rhythms by making sure you get sunlight early in the day and by avoiding blue light from your electronic devices too close to bedtime. Find out more on how blue light affects your overall health.

Your use of over-the-counter sleeping pills
You can find sleep aids on the shelves of your pharmacy that rely on diphenhydramine—it’s a commonly used drug for allergy and cold symptoms that also turns up in sleep aids. “Use of drugs in this same class [as diphenhydramine] has been associated with up to a 54 percent increased risk of dementia,” Hara says. So-called anticholinergic drugs block the action of a brain chemical called acetylcholine, which is involved in learning and memory.

You are not powerless
Stressing out about whether your sleeplessness will increase your risk of Alzheimer’s disease is counterproductive. Instead, troubleshoot your sleep issues to get a better night’s sleep. “Exercising during the day—but not too close to bedtime—promotes sleep and is also good for your brain,” Dr. Fillit says. It’s also a good idea to avoid eating too close to bedtime and limiting caffeine in the afternoon, as both can keep you up, he says.” For when you’re craving coffee, resort to this caffeine-free bevvy.

Know when to see your doctor
If your sleep loss is chronic, talk to your doctor about solutions—and remember that poor sleep is only one of the many factors that may contribute to cognitive decline and dementia risk, says Hara. There are many ways to reduce the risk for Alzheimer’s, including these steps for brain health: eating a healthy diet, exercising, alleviating stress, being social, stimulating your brain throughout life, and managing chronic illnesses. To reduce your risk of Alzheimer’s disease, be sure to incorporate some of these everyday habits into your life.
