
New horizons in human anatomy, chemistry, and genetics
Think space is the final frontier? Try the human body. There are so many incredible things the human body does every minute, some we don’t know about yet. In 2019, doctors and scientists made some surprising discoveries about a number of things happening in the human body, including how certain conditions develop, what amazing adaptations our bodies can make, and even why bones that once seemed to be going the way of the Dodo are now re-evolving back into more people’s skeletons. The full significance of these discoveries might not be known for years—after all, this year’s Nobel Prize in Medicine went to three scientists who figured out how the body’s cells adapt to oxygen levels way back in the late 1990s and early 2000s. Only time will tell how these latest discoveries will impact future technologies and treatments, but the possibilities are endless.

Humans can regrow cartilage
In a process that’s like a salamander regrowing its tail, humans have the ability to regenerate cartilage, according to a paper published in October 2019 in the journal Science Advances. “We found that human cartilage can repair, but does it best at the ankle, at an intermediate level in the knee, and at a low level in the hip,” says Virginia Byers Kraus, MD, PhD, a professor of medicine, orthopaedics, and pathology in the division of rheumatology at Duke University School of Medicine in Durham, North Carolina. This could be why wear-and-tear arthritis, or osteoarthrtis, more often develops in the hips and knees rather than the ankles. The researchers also found that molecules called microRNA, which are used to regenerate limbs in the salamander, control this repair process in human cartilage as well. “This is significant because it suggests that boosting these microRNA in human joints might be a new approach to treating osteoarthritis, the most prevalent type of arthritis in the US and worldwide,” Dr. Kraus says. In addition, someday this discovery may pave the way for regrowing other tissues, such as human limbs.
Check out these science-baked natural home remedies for arthritis pain relief.

Bodies move a year after death
Scientists still don’t know all the bizarre things that happen to your body after you die. However, in a discovery that could have implications for crime scene investigators, researchers using time-lapse photography found that bodies can move a great deal for up to a year after death. “During my study I expected to see some movement in the early stages of decomposition, for example when the abdomen bloats and with rigor mortis,” says Alyson Wilson, a forensic science student at Central Queensland University in Australia, who published her initial research on post-mortem time-lapse photography earlier this year in the journal Forensic Science International: Synergy. (Wilson says her latest research will be published in a forensic science journal by the end of 2019.)
“What the study found was that all the limbs of the body continued to move throughout the entire study of 16 months—this was an unexpected finding, and the amount of movement was astonishing,” she says. For example, arms positioned right next to the trunk of a body could move all the way out to the side. “As far as I am aware no studies have quantified human post-mortem movement,” she says. “Body position at time of death is vital for understanding the cause or circumstances surrounding the death, making any post-mortem movement of the remains highly significant for forensic investigations.”

There may be a “pain organ”
Believe it or not, scientists are even discovering entire new “organs” they didn’t know were inside the body—in this case, a mesh-like web of cells inside the skin that sense pain, according to research published in the journal Science in August. Contrary to the commonly-held notion that nerve endings detect pain, “our study shows that these nerves are ensheathed by a previously unknown cell type in the skin, which respond to painful stimuli and which can start the pain sensation,” says Patrik Ernfors, professor of medical biochemistry and biophysics at Karolinska Institutet in Stockholm, Sweden. These cells “form a web-like mesh together with nerves, building a sensory end-organ just underneath the outer layer of the skin that plays an active role in sensing harmful stimuli.” The finding could have important implications for chronic pain disorders. “This is something we are now studying, but don’t yet have an answer,” Dr. Ernfors says.

Your brain controls how you listen in a crowd
Ever wonder how your brain is able to focus on what one person is saying when you’re at a loud party or restaurant? In a discovery that could lead to advances in hearing aid technology, scientists figured out how your brain decides what sounds to focus on. The findings were published in October in the journal Neuron.“We can be in a noisy room filled with voices, yet we are able to shut out almost all of them, focusing only on the one person we are listening to,” says Nima Mesgarani, PhD, a neuroengineer at Columbia University’s Zuckerman Institute in New York. “We studied how different parts of our auditory cortex [the part of the brain that processes hearing] are involved in solving this challenging cognitive problem, and showed how the interaction between these regions gives rise to [selecting] the target speech.”

The brain can adapt to having a sixth finger
In more exciting findings about the brain, it turns out our noggins are even more flexible than we thought. In this study published in June in the journal Nature Communications, two people with six fingers (called polydactyly) were found to have extra abilities and skill in terms of object manipulation, rather than motor impairments. MRIs showed the brain actually figured out how to use and control the additional finger to its advantage. “Our subjects can use their extra fingers independently, either alone or together with the other five fingers, which makes manipulation extraordinary versatile and skillful,” Carsten Mehring, PhD, a professor of neurobiology and neurotechnology at the University of Freiburg in Breisgau, Germany, said in a statement. “For instance, in our experiments subjects can carry out a task with one hand, for which we normally need two hands.” The findings could have implications in the development of artificial limbs.

There are even more microbiome bacteria
Scientists are making new discoveries all the time about the surprising things your microbiome reveals about you. In the largest study of its kind, published in January in the journal Cell, researchers found thousands of new little bugs we didn’t know about before that make up the microbiome, the collection of “good” bacteria present in our body. “The human microbiome has been extensively studied for decades, yet there are still so many bacteria inhabiting our body that we have never seen, observed, and described before—in our work we performed a large-scale effort to catalog as many of these still elusive bacteria as possible,” says Nicola Segata, PhD, a computational biologist at the University of Trento in Italy. “There is clearly a lot of work still to do in the field of microbiome research, but our resource is now allowing us to survey much more comprehensively the composition of the human microbiome.” Identifying how the tiny microbes are linked with diseases could pave the way for new treatments, he says. (Psst: Here are a few expert-approved ways to improve your gut health this season.)

A tiny knee bone is back from the past
Why would a little knee bone that evolved out of the human body come back? That was the question that stumped researchers who, after looking at 21,000 knee studies over 150 years, discovered that the bone was present in only 11 percent of the population 100 years ago—but in 39 percent today. Their results were published in April in the Journal of Anatomy. “We found the fabella, a sesamoid bone [a bone inside a tendon] located behind the knee, is about three times more common today than 100 years ago—what makes this really strange is other sesamoid bones in the human body are just as common today as they once were,” says Michael Berthaume, PhD, a bioengineer at the Imperial College London in the UK. What could be behind the fabella’s return? “On average people are better nourished now than they once were, and better nutrition means people are heavier and have longer bones, meaning there is more force and torque around the knee when people walk,” Dr. Berthaume says. “As bone forms in response to mechanical stimuli, this increased force and torque at the knee may be causing the fabella to form.” This could also be why people with arthritis are more likely to have a fabella.
“In a time when most people claim gross anatomy is a ‘dead science,’ it is exciting to find that the human body is changing on such a drastic scale,” Dr. Berthaume says. “How often is it that we find the human body has an extra bone, one that was much less common a mere 100 years ago?”

There are genome areas for left-handedness
Why are some people left-handed? Researchers might have found out, revealing their discovery in the journal Brain in September. After analyzing the genomes of 400,000 people, the scientists found several genetic regions responsible for handedness, which were also linked with brain development and structure. “This research is significant as it gives clues to the fundamental biology of what leads to left-handedness in humans,” says Gwenaelle Douaud, PhD, an associate professor and Medical Research Council fellow at the University of Oxford in the UK. “This is the first time that left-handedness has been shown to be driven by the complex interplay of many genes that contribute to brain organization, particularly in the regions dedicated to language.”
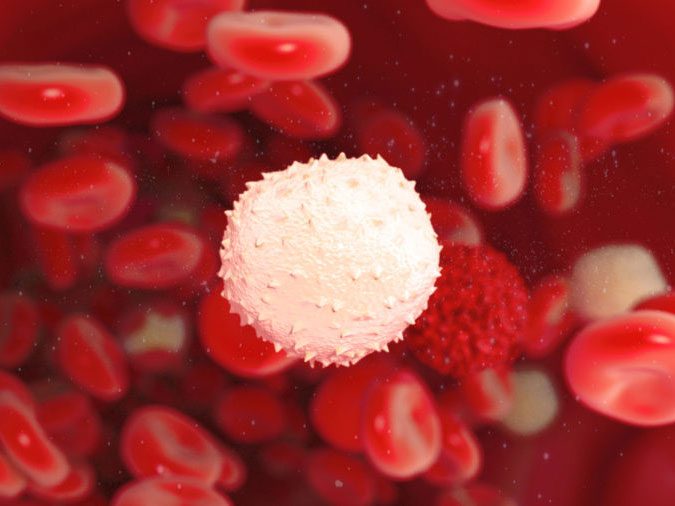
White blood cells help shape gallstones
Doctors have known what gallstones are made of—cholesterol and calcium salts, if you’re curious—for a long time. But they didn’t know exactly how everything was glued together, until a study published in September in the journal Immunity. Scientists examined “sludge,” fluid taken from human gallbladders. “We studied the formation of gallstones and found that white blood cells are responsible for the clumping of crystalline matter in the gallbladder,” says Martin Herrmann, PhD, an immunologist at the University Hospital Erlangen in Germany. “The clumped material then forms the more or less spherical aggregates, which appear as gallstones. The knowledge of this process could open up new treatment options for recurring gallstone disease in the future.” Keep in mind, these weird things happen to your body during the winter.

A brain biomarker is linked to suicidal thoughts in PTSD
People who suffer from post-traumatic stress disorder (PTSD) are much more likely to be at risk of suicide than the general population. But it’s not always easy to figure out who is most at risk, and how to treat them. But researchers who published a study on brain imagery in May in the journal Proceedings of the National Academy of Sciences may have uncovered a clue. “We detected that a location of a certain chemical might be different in brains of individuals with PTSD as compared to control or depressed individuals, and that this might relate to suicidal thinking in individuals with PTSD,” says Irina Esterlis, PhD, an associate professor of psychiatry at Yale. “Our work is important given that currently there are only two FDA medications that are approved for the treatment of PTSD, neither were developed specifically for PTSD and both take weeks to months to exert their benefits.” Plus, there are currently no FDA-approved treatments to help alleviate suicidal thinking in people with PTSD, she says. If manipulating this brain chemical is effective, the discovery “would be a substantial breakthrough and relieve suffering to many individuals and their families,” Dr. Esterlis says.

Fibromyalgia may be detectable in a blood sample
Some people still don’t believe the pain disorder fibromyalgia exists, and diagnosis in patients is difficult. But now, proof of the disease’s existence, as well as a way to treat it, may have been discovered. In a study published in March in the Journal of Biological Chemistry, researchers using a new method found a molecular signature for fibromyalgia that was reliably detected in blood samples, and that could present a new target for drugs to treat. “Fibromyalgia is a chronic pain disorder that results from abnormalities in central pain processing,” says Kevin Hackshaw, MD, rheumatologist at The Ohio State University Wexner Medical Center in Columbus. “The importance of this finding is due to the fact that fibromyalgia suffers from a lack of reliable therapeutic options. A reproducible, objective marker identifying fibromyalgia could confirm the presence of disease.” More research on a larger population is needed, but he hopes a blood test will be available within five years.

Humans can smell even without olfactory brain area
If you think you know how we smell—with our noses, of course—a study published in the journal Neuron in November suggests there’s more to it. The olfactory bulb is the brain structure thought to be responsible for processing smells, but the recent research found that two women without an anatomically defined olfactory bulb still had a great sense of smell even without it. (They did more research and estimate that about 0.6 percent of women may lack an olfactory bulb, but still have a normal sense of smell.) “Normal sense of smell in subjects without an olfactory bulb has powerful implications,” says Tali Weiss, PhD, of the department of neurobiology at the Weizmann Institute of Science in Rehovot, Israel. “These results suggest a reexamination of cause and effect regarding the lack of olfactory bulbs in congenital anosmia [the inability to smell].” Although the exact reason some people can smell without the olfactory bulb isn’t yet known, Dr. Weiss says one possibility is that brains can create a “smell map” outside of the olfactory bulb; or that “such maps are not completely necessary for the basic facets of human smell,” she says.

Defects in cell death may lead to autoimmune diseases
So much is yet to be learned about autoimmune diseases and the inflammation that may cause them. But in a study published in November in the journal Cell Reports, researchers discovered a protein in dying white blood cells that sends out “find me” and “eat me” signals to other cells that clear them away. (This is a normal process of programmed cell death that occurs to millions of cells every day.) But if this protein is faulty, the dead immune cells might not be cleared from the body. “Defects in this process trigger a wide variety of inflammatory disorders like autoimmunity,” Georgia Atkin-Smith, PhD, a biochemist at La Trobe Institute of Molecular Science in Australia, said in a statement. “Now, for the first time, we have a new insight into what may be the underlining cause of these diseases.”

The brain responds to a memory booster
Memory loss, as occurs with Alzheimer’s disease and dementia, may not be as permanent as we think. A study published in the journal Nature Neuroscience in April discovered that harmless electrical currents can stimulate the brain into working better. “We developed a new protocol for applying safe, noninvasive, and extremely weak electrical current to the human brain,” says Robert Reinhart, PhD, an assistant professor in the department of psychological and brain sciences at Boston University. Then, using this new method, they found they could make precise changes in how certain brain areas communicate with each other. “The result was a significant boost in brain plasticity—the natural ability of the brain to heal itself—and improvement in short-term memory performance for healthy 60- and 70-year old adults, with effects lasting longer than 50 minutes,” Dr. Reinhart says. “This research lays the basis for developing new drug-free neuroscience therapeutics for people with memory problems, such as those suffering from Alzheimer’s disease.”

DNA may only be one of many genetic molecules in the body
DNA is the building blocks of the human body, right? Yes, but it may not be the only one. You may have also heard about RNA, another nucleic acid, which helps the process of gene encoding along. But in a study published in the Journal of Chemical Information and Modeling in September, scientists using computational techniques found over a million more variants that could have played a role in heredity, had evolution not selected DNA for the task. These molecules, though, may suggest new genetic-based treatment for disease, and also call into question the evolution of life as we know it. “It is truly exciting to consider the potential for alternate genetic systems—that these might possibly have emerged and evolved in different environments, perhaps even on other planets or moons within our solar system,” Jay Goodwin, PhD, a biochemist at Emory University, said in a statement.
Medically reviewed by Jill Silverman, MD.
Next, check out these DNA tests to help determine your ideal diet and fitness plan.
