Too many women are dying from cervical cancer
An estimated 13,240 new cases of invasive cervical cancer were diagnosed in the United States in 2018, according to the American Cancer Society, and 4,170 women died from it. “These numbers should be much lower because we have a vaccine to prevent cervical cancer and a screening test that can catch it before it has spread,” says Kathy MacLaughlin, MD, a family medicine specialist at Mayo Clinic in Rochester, Minnesota.

Routine Pap testing every three years saves lives
Papanicolaou (Pap) smear tests, which involve swabbing a sample from the cervix to detect precancerous cells, can find changes in the cervix before cancer develops—or catch the cancer early when it’s easier to cure. Since Pap tests were introduced in the 1950s, the incidence of invasive cervical cancer declined dramatically: Cases and death rates declined by more than 60 percent since the 1960s, according to the National Cancer Institute. Unfortunately, the decline has tapered off over the last 15 years.

Or combination Pap test and HPV test every five years
Experts recommend Pap smear tests every three years for women 21 to 65 years. Another option for women 30 to 65 years is screening with a combination of Pap test and HPV test every five years. (This is called co-testing.) “This is what is recommended by all groups,” says Dr. MacLaughlin. “Routine screening every three years with a Pap test or every five years with a Pap-HPV co-test ensures precancerous changes are caught early and may be followed more closely or treated.”

Cervical cancer screening rates are still too low
Less than two-thirds of women ages 30 to 65 were up-to-date with cervical cancer screenings in 2016, according to a study in the Journal of Women’s Health. The percentage is even lower for women 21 to 29, says study author Dr. MacLaughlin.

There’s a shot that can prevent most HPV-related cancers
HPV, short for human papillomavirus, is actually a group of more than 200 extremely common viruses. Some types of HPV are sexually transmitted and can cause genital warts. Others can lead to penile cancer in men and cervical, vaginal, and vulvar cancer in women. Men and women can also develop oral, anal, or rectal cancer from HPV infection. The Food and Drug Administration (FDA) has approved three vaccines that can prevent infection by the types responsible for 70 percent of cervical cancers—and an even higher percentage of some of the other HPV-caused cancers, according to the American Cancer Society. Don’t fall for these myths about HPV that could seriously damage your health.

HPV vaccines are given as a series of two or three shots
The federal Centers for Disease Control and Prevention (CDC) recommends that kids who are 11 or 12 get two shots of the HPV vaccine six to 12 months apart. Adolescents who receive their two shots less than five months apart require a third dose. Children older than 14 years need three shots, given over six months. Three doses are also recommended for anyone age 9 to 26 who has a challenged immune system.

The HPV shot is not just for teens and tweens
The FDA recently recommended HPV shots for men and women aged 27 to 45. The ideal time to get vaccinated is still before you become sexually active, however there are benefits to being vaccinated later in life too, Dr. MacLaughlin says.

HPV doesn’t always cause cancer
HPV is a very common virus. About 14 million people, including teens, become infected each year, according to the CDC. Most people never develop symptoms, and the HPV infection often clears up on its own, Dr. MacLaughlin says. “On the one hand, this is the most common STD and anyone who is sexually active will be exposed, but most people won’t have a problem,” she says. “It’s a small percentage of people where HPV will stay and cause problems.”

Women under 30 don’t need HPV testing
Women under 30 don’t need the HPV test with the Pap test, according to the Canadian Cancer Society. But such testing may be used in this age group after an abnormal Pap result. Co-testing is preferred in women 30 and older. Talk to your doctor to make sure you are getting the right cervical cancer screening tests for you based on your age and any personal risk factors.

Too few kids get the HPV shots
Yes, HPV vaccinations have increased in recent years, but they are still too few, according to a 2018 report from the President’s Cancer Panel. The percentage of kids starting the HPV vaccine series increased an average of 5 percent a year between 2013 and 2017, however less than half of teens were fully vaccinated as of 2017, the report states. Many parents have felt uncomfortable with the vaccine, as HPV is sexually transmitted and parents don’t want to (or can’t) think about their 11-year-old having sex at some point in the future, Dr. MacLaughlin says. But that’s the whole point: “You want to give the shot before someone becomes sexually active. This is the time that the body can mount the most robust immune response to HPV.”

Boys should get the HPV shot too
The HPV shot is recommended for girls and boys, but one in five parents of adolescent boys reports that they do not plan to vaccinate their son because they did not get a recommendation to do so—compared to one in 10 parents of adolescent girls, reports Anna Beavis, MD, a gynecologic oncologist fellow at Johns Hopkins University. “In general, the most common reason parents do not vaccinate both boys and girls is a misperception that the HPV vaccine is not necessary,” Dr. Beavis says. (FYI: These patient habits that bother gynecologists.)

Seniors do still get cervical cancer
One in five women older than 65 is diagnosed with cervical cancer, according to a 2018 study presented at an annual meeting of the Society of Gynecologic Oncology. Despite this, it is recommend that cervical screening stop after women turn 65. The study authors disagree, explaining that their data suggests that patients are being aged out of screening too soon. Testing is recommended for women over 65 if they’ve had cervical abnormalities or cancer in the past. If you’re at this age, discuss your potential screening concerns with your doctor.

You might not have cervical cancer symptoms until it’s advanced
Once symptoms appear, cervical cancer has likely begun to spread: Symptoms of advanced cervical cancer may include abnormal vaginal bleeding, such as bleeding after sex, an unusual discharge from the vagina, and pain during sex, according to the American Cancer Society. Other symptoms such as the frequent or urgent need to urinate, fatigue, and unexplained weight loss. While there are many non-cancerous reasons for these symptoms, it’s always better to get checked out by your doctor.

Smoking makes matters worse
“Smoking lowers the chances that your body will be healthy enough to clear HPV on its own,” says Dr. MacLaughlin. Smoking aside, here’s what causes lung cancer.

IUDs may help prevent cervical cancer
IUDs may reduce your risk of cervical cancer by about a third, according to a report published in the journal Obstetrics & Gynecology. Researchers hypothesize that when the device is inserted, the body may mount an immune response to it as a foreign agent and that immune response may also clear HPV.
Find out if an IUD is the right birth-control method for you.

Cervical cancer treatment is improving
The five-year survival rate for women diagnosed with cervical cancer is close to 75 percent today, according to the National Institutes of Health. Most of the time, treatment involves radiation plus chemotherapy.

Cervical cancer can be one reason for a hysterectomy
There are many reasons that a doctor will perform a hysterectomy (the surgical removal of the uterus), and cervical cancer is one of them.

There are risk factors for cervical cancer
Having a compromised immune system, having sex for the first time at an early age, having multiple sex partners, taking birth control pills for more than five years, and testing positive for HIV all increase risk for developing cervical cancer, says Stephanie V. Blank, MD, director of the Division of Gynecologic Oncology for the Mount Sinai Health System, Icahn School of Medicine at Mount Sinai.

There is more than one type of HPV shot
The FDA gave a nod to two HPV vaccines: Gardasil and Cervarix. These vaccines prevent infection with high-risk HPVs that cause about 70 percent of cervical cancers. Gardasil also prevents infection with HPV types that cause 90 percent of genital warts. “These vaccines offer an amazing opportunity—the possibility of preventing a deadly cancer,” Dr. Blank says.

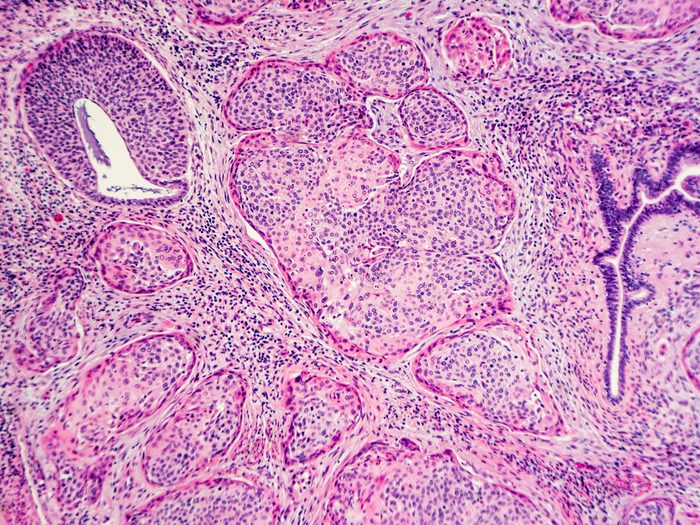
AI may one day diagnose cervical cancer
A computer algorithm that analyzes digital images of a woman’s cervix can accurately identify precancerous changes that require medical attention. In a study published in JNCI: Journal of the National Cancer Institute, the researchers report that computer analysis of the cervical images was better at identifying precancer than a human expert reviewer of Pap tests under the microscope (cytology). The new method may be valuable in areas where there is a shortage of health care providers.

New epigenetic screening test may top Pap, HPV tests
A new test for cervical cancer detected all of the cancers in a trial of 15,744 women, outperforming both the current Pap smear and HPV test, and it cost less, according to a study led by researchers at the Queen Mary University of London that was published in the International Journal of Cancer. This new test looks at so-called epigenetic profiles—the biological mechanisms that switch genes on and off. By contrast, the HPV test only identifies whether a woman is infected with cancer-causing HPV, not her actual risk of cancer. As such, the new test can better predict which women with HPV will go on to develop cervical cancer during the next five years. “The new test is much better than anything offered in the UK at present but could take at least five years to be established,” the study authors note.

Out-of-balance vaginal bacteria may be linked to cervical cancer risk
Women with cervical cancer or precancer have different vaginal bacteria populations than women who don’t have cervical tissue problems, according to a paper in NatureResearch: Scientific Reports. Researchers led by the University of Arizona Cancer Center’s Melissa M. Herbst-Kralovetz, PhD, associate professor at the UA College of Medicine-Phoenix, looked at 100 premenopausal women to find links between vaginal bacteria and cervical cancer. The research revealed that in cancer and precancer patients, lactobacilli—good bacteria—are replaced by a mixture of bad bacteria. As Lactobacillus populations decreased, cervical abnormalities became more severe.

The risk of dying from cervical cancer is higher than women realize
The rate of deaths from cervical cancer is actually higher than we thought. According to a study from the Johns Hopkins Bloomberg School of Public Health in Baltimore, the original rate was flawed. “Prior calculations did not account for hysterectomy,” says study author Anne F. Rositch, PhD, MSPH, an assistant professor of epidemiology at Johns Hopkins Bloomberg School of Public Health. Although this doesn’t mean more women are actually dying than previously thought, it does mean that the chance of dying among the women at risk is greater. For white women in the United States, the new estimates are 4.7 women per 100,000, 47 percent higher than the previous estimate of 3.2; for black women, the rate is 10.1 per 100,000, 77 percent higher than the previous estimate of 5.7.

African-American women are more likely to die of cervical cancer
The Johns Hopkins study also found that black women are dying of cervical cancer at twice the rate as white women in the United States.”We already have national and state-level data to suggest that black women are less likely to receive adequate therapy at initial diagnosis [for cervical cancer], but we need to determine actionable reasons why care is differential to begin to address the mortality difference,” Dr. Rositch says. If you are African-American, make sure you’re getting regular screenings.

Low levels of vitamin D may play a role in cervical cancer
When a person’s levels of vitamin D dip, they’re at higher risk of a range of health problems—including cervical cancer. In one study, women with lower levels of D had a much higher risk of developing high-risk human HPV infection. Vitamin D is known as the sunshine vitamin because our bodies produce it in response to sunlight. If you live in a climate with long winters, talk to your doctor about supplements. (Here’s more on how vitamin D can benefit your health.)
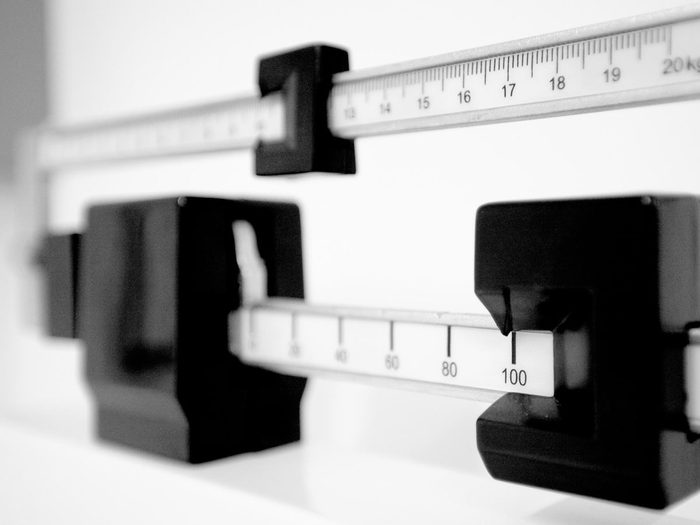
Your weight may affect your cervical cancer risk
Women who are overweight and obese may have a higher risk of cervical cancer compared to normal-weight women. Part of the reason may be that cervical cancer screenings are less effective in overweight women, suggests a study in the Journal of Clinical Oncology. The sensitivity of both HPV and Pap testing may be compromised in overweight or obese women, and doctors may be unable to fully visualize the cervix to see if a biopsy is needed.

You don’t have to get cervical cancer
This is one cancer that is preventable. “Between the HPV vaccine and improved screening options, which allow us to detect abnormalities before they turn into cancer, we have the tools to eradicate cervical cancer,” Dr. Blank said. “It is crucially important that we use these tools properly.”
Next, find out which household products may be linked to breast cancer.
