Why the confusion about HPV myths?
Some might think that the human papilloma virus (HPV) is a fairly new term. Well, it’s fairly new to the public, and that could be the reason for HPV myths spreading like news.
It was discovered in 1956 (somewhat new-ish), but it was 1984 when the sexually transmitted virus was linked with cervical cancer, according to Austin Community College. And with most things that are newly discovered, there is a lot of misinformation mixed with hints of credible research.
To clear up some confusion around HPV, we connected with Toronto-based Dr. Vivien Brown, past president of the FMWC. She was helping to promote Cervical Cancer Awareness Week (October 16 to 20), led by the Federation of Medical Women of Canada. The campaign offers more than 100 free pap clinics across Canada.

Like any STD, women should get regularly tested for HPV
Your Pap test is all you need to do regularly.
The expert says: “HPV is so common that about 80 per cent of adults in North America will have it at one point or another in their lives,” says Brown. “Most of us will clear an HPV infection on our own — you can have the virus and clear it a day later — so there is no benefit to testing for it on an ongoing basis. Persistent HPV infection is what leads to cancer, and a PAP test will show us there’s an abnormality.”
HPV is only transmitted through heterosexual sex
Nope. Not even a little bit true.
The expert says: “Unfortunately, HPV is transmitted through intimate touching so you don’t have to have intercourse to get it,” says Brown. “HPV is passed through moisture and contact, so you can have it on your fingertips, and it happens to same-sex and heterosexual partners.”

If a woman discovers she has HPV, her partner should be tested
Remember when Lena Dunham’s character Hannah on Girls told her ex about her HPV diagnosis? Turns out there is no shame with HPV as it’s very common. Not as common as the common cold, but many do have it.
The expert says: “There is often nothing to test in her partner as HPV can take weeks, months or even years to present itself,” says Brown, adding: “Remember, most HPV infections are cleared on their own. If a woman discovers she has HPV, there should be a discussion about decreasing her risk and her partner’s risk of developing oncogenic or cancerous HPV by vaccinating both partners.”
“According to the National Advisory Committee on Immunization (NACI), there is no upper age limit for HPV vaccination. The HPV vaccine is very effective for females and males of all ages, and those with previous exposure to HPV or a history of HPV-related diseases still benefit from HPV immunization.”

You’ll know if you have HPV
You won’t feel HPV and you won’t even “feel” having it.
The expert says: “Even the most dangerous strains of HPV will cause no symptoms,” says Brown. “You will only know if you’ve had an abnormal PAP test or genital warts — and you could have HPV without either.”

The vaccine has not been tested for safety over the long term
The vaccine is safe, report the most credible health organizations in the world.
The expert says: “This is a myth. We now have 10 years of experience with the vaccine, with more than 40 million doses given worldwide that show excellent long-term efficacy and safety,” says Brown. “The World Health Organization (WHO), Health Canada and the Center for Disease Control and Prevention (CDC) all agree on the safety of the vaccine.”

Having the vaccine means that it’s okay to have unprotected sex
Safe sex is always a concern, and we should never take our sexual health – and our health – for granted.
The expert says: Having the vaccine lowers your risk of HPV infection by 90 per cent, but unprotected sex puts you at risk for other STIs like chlamydia, herpes and gonorrhea.
Check out: Can You Get an STI From a Brazilian Wax?
If you use protection, you won’t get HPV
HPV is not the same as most sexually transmitted infections (STIs).
The expert says: As much as condoms decrease risk of pregnancy and infections other than HPV, HPV lives on skin so condoms don’t protect you from it. HPV is also really tiny and can get through the pores in a condom.
This is why regular checkups with your doctor are important.
Have you read this? 15 Things Your Gynecologist Secretly Wants to Tell You
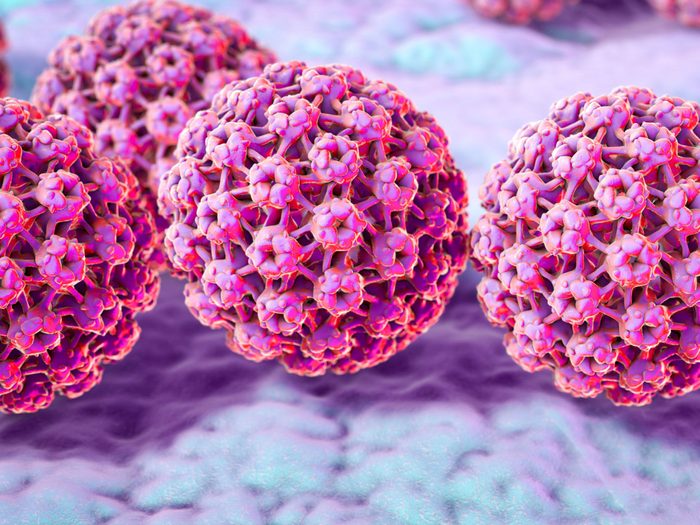
HPV means you will get cancer
It’s true, as we said in the beginning of this story, that HPV is linked to cervical cancer – but having HPV is not a predictor of the disease.
The expert says: “Thankfully this isn’t true,” assures Brown. “80 per cent of us will clear an HPV infection on our own. It’s only persistent HPV infections from certain sub-types of HPV that can lead to cancer.”
What is said about cancer causes can be confusing. That’s why we wrote this: Stop Believing The BS – 10 Cancer Myths Busted
The number of sexual partners you’ve had is telling of your risk for HPV
Risk has nothing to do with your sexual history.
The expert says: “You can get HPV from a single partner, and that partner could be carrying cancer-causing HPV,” says Brown.

Only young women get HPV
Although the age for vaccination is young (11-12 years of age) in Canada, it’s not limited to girls in this age group.
The expert says: “This is also untrue; everybody is susceptible to HPV and it’s not related to age,” says Brown. “It’s more related to your sexual partners, no matter if you’ve had one or many of them.”
Check out: Why Sex Can Be Dangerous For Middle-Aged Canadians
