
The most widely consumed beverage in the world, after water, is tea. And it’s not surprising. A cup of tea is easy to make, satisfies your tastebuds and delivers a type of warmth most comparable to a hug. But there’s another reason so many Canadians continue to enjoy the beverage year after year. The whole teatime process—from letting the tea bag steep to breathing in its warm aroma—can help you be more mindful.

The practice of mindfulness is steeped in health benefits. It can help relieve stress, improve mental health, boost heart health, lower blood pressure, improve sleep, soothe gastrointestinal issues and minimize chronic pain. Mindfulness was the goal behind Tetley’s new line, Live Tea. It was specially formulated with good-for-you herbs to help you be more present every day. Through enticing flavour profiles, the teas can wake up your senses, sparking feelings of joy and encouraging a moment of calmness.

Ready to connect with yourself, tune in to your surroundings and live a life that’s authentically yours? Here are the three teas from Tetley’s new Life Tea line that will help you do just that.
Live Bold Tea – Cinnamon, Chai & Rooibos
If you like tea that packs a mouthful of bold flavours, this one’s for you. Tetley’s Live Bold Tea features a superstar blend of ingredients including cinnamon, chai and rooibos.
Cinnamon isn’t just a spice that makes apples, oatmeal and baked goods so much better. It can offer health benefits, too. One study found participants on insulin therapy who consumed cinnamon saw a reduction in blood sugar levels, and other studies found daily consumption of cinnamon lead to a significant decrease in bad cholesterol. If that’s not enough, the herb also contains antioxidants, which can reduce the risk of heart disease and soothe inflammation.
The chai in Tetley’s Live Bold Tea is made up of herbs including ginger, cardamom and cloves—all of which have health perks. Ginger contains vitamin C and some B vitamins, cardamom contains potassium, magnesium and calcium, and cloves contain folate, calcium and potassium.
The last star ingredient, but certainly not the least impressive, in Live Bold Tea is rooibos. Like cinnamon, it has high levels of antioxidants, which help to promote heart health. Since rooibos is this tea’s base, it’s naturally caffeine-free.
Live Bold Tea – Cinnamon, Chai & Rooibos, $3.99, tetley.ca
Live Calm Tea – Chamomile, Spearmint & Orange
If you prefer your tea to boast a soothing taste, try Tetley’s Live Calm Tea, which features a blend of chamomile, spearmint and orange.
Chamomile is frequently enjoyed before bed, as its delicate taste encourages feelings of serenity—but that’s helpful for any time of day, too. The flower is often used to aid digestive issues, helping to soothe indigestion, diarrhea, nausea and gas.
Similarly, spearmint can also help alleviate digestive problems, but does so by relaxing stomach muscles. It can tame feelings of nausea, treat indigestion, relieve cramps and soothe a sore throat.
Lastly, orange, an antioxidant, can offer a zesty taste and scent that may help lift your mood and reduce stress.
Like Live Bold Tea, Live Calm Tea is also caffeine-free, making it perfectly suitable to enjoy before catching some Zzzs.
Live Calm Tea – Chamomile, Spearmint & Orange, $3.99, tetley.ca
Live Cool Tea – Peppermint & Spearmint
For a tea that’s super refreshing (and leaves your breath fresh, too) try Tetley’s Live Cool Tea. Its delightful blend of peppermint and spearmint is sure to help you unwind and not give you the jitters as it’s also naturally caffeine-free.
Peppermint can help improve digestion and has been shown to help boost memory. It also has antibacterial properties and can help improve headaches, offer decongestion and relieve allergy symptoms. This herb can also help relax muscles, which can aid in your pre-bed ritual.
Spearmint, as mentioned above, can help relax the stomach. This means Live Cool Tea can help your whole body unwind, setting you up for a restful sleep.
Live Cool Tea – Peppermint & Spearmint, $3.99, tetley.ca
Visit Tetley.ca to learn more about their new Live teas.
Since being diagnosed with breast cancer in May of this year at age 70, beloved fashion journalist Jeanne Beker has been candid about her journey. Canadians know her as the stylish icon from Fashion Television, and Beker has been focusing on staying positive and making others less afraid of cancer. Beker started chemotherapy earlier this year and has since been documenting it all—from losing her hair, to the kind nurse who preps her for chemo, to the rigamarole that is a mid-treatment pee break—for her followers on Instagram.
We spoke to Beker about her diagnosis, her support system and how she’s staying upbeat.
What was the diagnosis process like?
I had just had a routine mammogram—I go every two years, though I wish I had been going every year because I didn’t know that people with dense breasts really have to be checked a lot. So, a couple days after my mammogram, my doctor called and said they had discovered something. I had been feeling totally normal—fine, perfect. I never felt anything lumpy in my breasts or anything. They called me back for a biopsy and an ultrasound and MRI. Then I got that call that changed my life—that call that nobody wants to get. Those first few days, as anyone can attest to, were incredibly dark and very scary because you don’t know exactly what’s going on and how bad it is, or if they can treat it. It’s just awful, and you go down 5,000 rabbit holes.
What happened next?
I got an appointment with a doctor at the breast clinic of Princess Margaret Cancer Center. She’s a surgeon, and she immediately made me feel better by telling me that the prognosis is good and the cancer had been caught early. I had to see the oncologist the following week, who’s another rock star—they’re all rock stars at Princess Margaret. The oncologist told me it’s not only treatable, it’s curable. When I heard that, I just felt so relieved. He told me about three different treatment options, and I decided to do 12 rounds of Taxol [a form of chemo], followed by surgery and radiation, because it was a bit easier to maintain my lifestyle with that treatment route. I’m glad I went that way because it was quite tolerable, and I’m done chemo. My surgery will happen later in October.
I’m hanging on and feeling very positive and very grateful. When I was growing up, most people [with cancer] had really bad outcomes. But the landscape has changed. Research, especially in the field of breast cancer, has progressed to such a brilliant degree. Things are changing all the time. So I just feel incredibly lucky. There’s been so many silver linings to this journey as well.
View this post on Instagram
Tell me about those silver linings?
One of them has been my Instagram. Social media can be the root of all evil, but when used correctly, it can also be an incredible way to communicate and touch people and be touched by people. When I decided to go public with my journey, it wasn’t a big decision at all. I was like, of course I’m going to put it on my Instagram because I’m all about authenticity. And this is something very real that I’m living with. It’s something that I know affects so many women—one in eight women are going to be diagnosed with breast cancer in their lifetime. Why wouldn’t I want to reach out and tell people who have been watching me and supporting me all these years? I felt I owed it to them—and I owed it to myself—to be that open and honest.
I just actually held the hand of a very dear friend of mine who, for about a year and a half, went through her own cancer journey. It was during the pandemic and she was very alone. She didn’t want to tell anybody. She’s not a public person, so I understand wanting privacy, but I thought at the time that I would never be able to do that. It was just too much of a burden.
So, I started telling people about my diagnosis and the response [on social media] has been phenomenal. The positivity that I was getting back was phenomenally heart-swelling and my spirits were so lifted. Even if they just sent emojis, it was just such a joy to me.
(Related: What Doctors Want You to Know About Breast Cancer)
How have your friends and family supported you since the diagnosis?
All my friends have been fantastic. They’re always texting, emailing, calling, checking up on me. Even people I didn’t think I was very close to were asking if there was anything they could do for me. If I needed someone to pick me up for treatment, or go with me to the hospital—that kind of support was just so nice. But I think most importantly, my daughters have been great. My youngest daughter lives in the Yukon and drove all the way out here to be with me. And my other daughter lives nearby and she’s just been fabulous. My sister in LA has been incredibly supportive and positive. Even though I’ve just spoken to her on the phone, she’s offered to come here.
And, first and foremost, my partner. We’ve been together for seven years. He was with me when I got the phone call and without skipping a beat, he said, “Don’t worry, we’ll get through this together.” He comes to all my doctor appointments with me. He’s just my biggest cheerleader, and I’m so lucky to have that kind of support. And then I’ve got my big goldendoodle dog who acts as a therapy dog. He just just comes and cuddles me whenever I need it. I am really looking forward to the [CIBC Run for the Cure] on Sunday, where I’ll talk and meet with other women with breast cancer.
Tell me a bit about your advocacy work around the Canadian Cancer Society CIBC Run for the Cure.
The community of women that you find [after you’re diagnosed] is phenomenal. You feel like you’re in some kind of special club with these women. Granted, it’s a club that you may not have wanted to be part of, but once you’re in it, everybody is so supportive of one another. It’s such a wonderful feeling to know that you’ve got so many hands to hold. I think the whole event is just so incredibly inspiring, besides the fact that it raises so many funds.
What do you hope that people learn from your story?
I hope that women become aware of the fact that they better go for a mammogram on a very regular basis. I think a lot of women put it off because it’s not a pleasant experience. But it’s really important to go in!
And, I want to remind people to live your life to its fullest, as much as you can—and appreciate every glorious second of it. I’ve never savored life more. I mean, the whole diagnosis just made me realize how much I was in love with my life. All of a sudden, the world seems like an even more beautiful place. I really hope to be able to stick around for a lot longer.
This interview has been edited and condensed.
Next: How to Do a Self Breast Exam
When Vancouver-based mom and software project manager Mona Stilwell gave birth to her twin boys in 2014, her mother hired a Taiwanese private chef (who also happened to have a nursing background) to make sure Stilwell ate nutritious food as she recovered from giving birth. Every day for a whole month, Stilwell received a delivery of three healthy, hearty and traditional meals that were meant to help her heal after giving birth. “I was so busy and freaking out over having twins that I didn’t even think about food,” says Stilwell. “As I entered my third trimester, my mom basically told me that she had hired this person and I couldn’t say no.”
It wasn’t until she went back to work the following year that she realized how many new parents wished they could receive the same kind of support. There are postpartum traditions around the world centred around community care within villages and families, but “it wasn’t put into a consumer-packaged service,” Stilwell says. So, in 2018, she launched Feeding Mama to provide new moms in the Vancouver area with delicious and nourishing meal deliveries that follow the traditional Chinese practice of “sitting the month.”
Sitting the month, or zuò yuè zi, is a form of postpartum care followed by practioners of Traditional Chinese Medicine (TCM). The practice has been traced as far back as the year 960 and there are documents from over 2,000 years ago that highlight postpartum care rules that have been passed down for generations. Typically, postpartum mothers are taken care of by their relatives: grandmas, moms, and aunties help with everything—including household tasks and childcare—so the new mom can focus only on resting and recovering.
“You basically don’t leave your home for 30 days, you don’t take care of all the [other] children, you’re not cooking, you’re not cleaning the house, you’re not taking a shower, you’re not getting your hair or body wet, and you have to eat warm foods,” explains Stilwell.
These rules all stem from TCM—hair washing, for example, is forbidden because, it’s believed, you might catch a cold. (It’s also why having a fan or the air conditioning on is a no-no.) There are also specific, traditional dishes that are meant to be eaten, containing ingredients like ginger, chicken, or liver to boost health and fulfill nourishment needs. Foods that are anti-inflammatory and full of iron, protein, and vitamin C are emphasized—the first to help replenish iron lost from bloodshed during childbirth and in the weeks that follow, and the rest to provide energy for a lactating parent who may be up at all hours, consoling the baby and nursing or pumping.
Stilwell grew up in Richmond, B.C., but she was born in Malaysia and her mother’s family was from China and her dad’s family was from Macau and Portugal. This blending of cultures has influenced her business: Feeding Mama uses traditional ingredients, and also leans on modern nutritional sciences to design and deliver meal plans to new parents in the greater Vancouver area—from broths, teas, and lactation cookies to dinners of steamed salmon with bok choy and ginger rice quinoa. Feeding Mama’s soups and meals are chock-full of ingredients like lentils (which are high in iron) and sweet potatoes (which have a ton of vitamin C).
“I grew up in a very Chinese family, so many of the things we eat are for function, even though it’s bitter—like Chinese medicine is the most horrible-tasting thing you can consume, but it’s good for you,” she says. “So, I thought, there must be a way to make very functional foods really tasty and incorporate more of the foods I’ve been exposed to as a foodie growing up in Vancouver.”
Aside from providing clients with delicious and nutritious meals, Stilwell also hopes to bring a community care aspect to the business. “Every time I send a delivery, I write a little note of encouragement,” she says. “Things like ‘your recovery matters,’ ‘be gentle with yourself’—things I wish someone had said to me in a non-judgmental, unconditional love kind of way.”
Often, new parents don’t—or can’t—allow themselves much time to rest. They aren’t prepared for how relentless newborn care is, Stilwell says, and the grandparents often forget how hard the early days were: It can be difficult to feed yourself well if you’re trapped under a nursing or sleeping baby, or when you often only have one hand free. Simply getting to a grocery store with a newborn who’s sleeping-and-feeding-and-pooping in two-hour increments, around the clock, can feel logistically impossible. Plus, parents may live far away from their relatives or don’t have the space to accommodate long family visits, so there isn’t anyone to help cook meals for them.
This is where a service like Feeding Mama can step in. And while the practice of sitting the month has existed in China and the Chinese diasporic community for a thousand years and similar practices are common in other East Asian cultures, Stilwell believes that there’s room to adapt the tradition for all parents. “It’s a tradition, but the food is not traditional,” she says.
Signature meal plans start at $200 (and can cost as much as $2,600, depending on how many meals you want, and for how long). Gift cards from $25. feedingmama.ca
This story is part of Best Health’s Preservation series, which spotlights wellness businesses and practices rooted in culture, community and history. Read more from this series here:
Meet Sisters Sage, an Indigenous Wellness Brand Reclaiming Smudging
This Canadian Soap Brand is Rooted in Korean Bathhouse Culture
Sharing Chinese Herbal Soups and Teas, Steeped in Tradition
Get more great stories delivered straight to your inbox by signing up for the Best Health Must-Reads newsletter. Subscribe here.
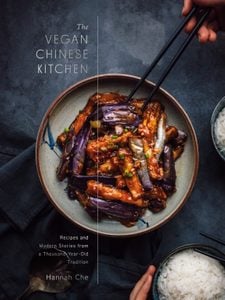
Although taro is often associated in the West with creamy sweet drinks and desserts, its delicious appeal is most obvious in savory dishes. The purple-mottled flesh cooks down to fragrant, meaty bites with a fine-textured starchiness, a quality called 麵 miàn, or “floury,” and a stick-to-the-roof-of-your-mouth savoriness reminiscent of a hard-boiled egg yolk. This was one of my favorite menu items at Gudian Meiren, a vegetarian restaurant in Taipei, where it was featured alongside other dishes like seitan “ribs” skewered on sugarcane with a tangy hibiscus reduction, braised tofu with bamboo shoots, and crisp roast “duck” on a bed of puffed rice. You won’t find coconut milk used traditionally in most regional Chinese cuisines (with the exception of Hainanese), but the influence of South Asian cuisines on modern Chinese cooking can be seen in the growing popularity of dishes with coconut milk, like this one.
(Related: You’re Seriously Underusing Your Rice Cooker)
Coconut Clay Pot Taro & Edamame
Yēxiāng yùtóu bāo
椰香芋頭煲
Serves 4
Ingredients
- 4 large dried shiitake mushrooms
- 1 cup (240 mL) boiling water
- 1 medium (10 ounces / 280 grams) taro root
- 3 tablespoons Shallot Oil or vegetable oil, divided
- 1 (2-inch) piece (15 grams) ginger, unpeeled, washed and thinly sliced
- 3 garlic cloves, minced
- 2 tablespoons fermented soybean paste
- 1 cup cooked shelled edamame, thawed if frozen
- 1 cup (240 mL) unsalted stock of any kind or water
- ½ cup full-fat coconut milk
- 1 tablespoon sugar
- ½ teaspoon kosher salt, plus more to taste
- ¼ teaspoon ground white pepper
- Handful of fresh cilantro, both stems and leaves finely chopped
Directions
In a small bowl, cover the mushrooms with the boiling water and place another bowl or plate on top to weigh them down. Soak for 30 minutes.
Meanwhile, peel the taro and cut it into 1-inch cubes. In a skillet or wok, heat 2 tablespoons of the shallot oil over medium-high heat until shimmering and then add the taro. Sear the taro in the hot oil, flipping occasionally, until golden brown on the edges, about 4 minutes.
Remove from the pan.
Drain the shiitake mushrooms, reserving the soaking liquid, snip off and discard the stems, and cut the caps on a diagonal into 3 or 4 thin slices each. Set a clay pot on or return the wok to the stovetop over medium-low heat and heat the remaining 1 tablespoon shallot oil until it shimmers.
Add the ginger and mushrooms and stir-fry until the edges of the mushrooms start to brown and stick, about 3 minutes. Add the garlic and fermented bean paste and stir-fry until most of the moisture has sizzled out of the paste and it smells delicious, about 20 seconds. Add the cooked taro and edamame, then pour in the stock and coconut milk. Season with sugar and salt to taste—this will depend on the saltiness of your soybean paste.
Cover and cook for 15 to 18 minutes, until the taro has absorbed most of the liquid and is completely cooked through and fork-tender. Add the white pepper, top with the cilantro, and serve immediately.
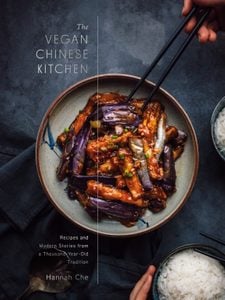
Excerpted from The Vegan Chinese Kitchen by Hannah Che. Copyright © 2022 Hannah Che. Photographs by Hannah Che. Published by Appetite by Random House®, a division of Penguin Random House Canada Limited. Reproduced by arrangement with the Publisher. All rights reserved.
Next: Shake Up Your Lunch With This Napa Cabbage & Vermicelli Salad
In the past, only vegetarians and vegans cared all that much about plant protein. That’s not the case anymore. In the first four months of 2020, sales of plant-based meat spiked 148 percent over the year before, according to the Plant Based Foods Association.
The plant-based food trend shows no signs of slowing down. By 2027, plant-based protein sales in the United States are projected to rake in 17 million dollars, more than triple today’s revenues, according to a report by Research and Markets.
So, what’s driving the plant-based protein craze and should you be getting more protein from plant sources versus traditional sources of protein, like meat, fish, eggs, and dairy? Here’s everything you need to know about plant-based protein.
What is a plant-based diet?
A whole food plant-based diet focuses on eating foods mainly derived from plants. These include a variety of fruits and veggies, whole grains (oats, brown rice, and quinoa), pulses (beans, lentils, peas, and chickpeas), nuts and seeds, herbs and spices, and occasional animal-based foods.
Those who follow a plant-based diet aren’t necessarily vegan or vegetarian. Rather, they’re opting to add more plant foods to their diets, and eating less processed foods and meat.
How it is different from vegan and vegetarian diets?
There are many similarities between a plant-based diet and a vegetarian or vegan diet. The main difference is that those following a plant-based diet might occasionally eat some animal-based foods. One follower of this diet may opt to eat one non-plant ingredient, such as fish. Another plant-based dieter may choose to occasionally eat meat.
Meanwhile, a vegan diet primarily consists of veggies, fruits, whole grains, pulses, nuts, and seeds (ideally), although any foods free of animal products or ingredients qualifies as vegan. Vegans avoid all animal-sourced foods and ingredients, even honey, gelatin, and collagen. Similar to vegans, those who follow a vegetarian diet will have no meat, poultry, or seafood. But vegetarians, like some plant-based eaters, can consume dairy and eggs. People who follow other forms of vegetarianism may eat fish and seafood.
(Related: 5 Meal Prep Tips for People Who Are Vegans or Vegetarians)
What is plant-based protein, anyway?
Protein does lots of great things for our bodies. In addition to building muscle and keeping us full between meals, protein helps build bones, hormones, antibodies, and more. Some of the best sources of protein include meat, poultry, fish, eggs, and dairy. But plants like beans, soy, nuts, seeds, and even whole grains pack surprising amounts of this nutrient.
Plant protein vs. animal protein
Animal foods offer complete protein. That means they contain all the essential amino acids the body needs to manufacture its own protein supply. Plants, on the other hand, often contain incomplete protein, which lacks one or more essential amino acids. There are exceptions, though. Both soy and quinoa are complete proteins.
For years, nutrition experts believed the only way to obtain enough essential amino acids from a plant-based diet was to combine plant proteins at meals, like eating rice with beans. In doing that, the theory went, you’d get certain amino acids from the rice and other amino acids from the beans.
Now, the thinking has changed. “Our bodies are quite sophisticated, and we now know that as long as we eat a variety of foods throughout the day, we can get the right proportions of amino acids from plants,” says dietitian Vandana R. Sheth, RDN, author of My Indian Table: Quick & Tasty Vegetarian Recipes.
Can you really get enough protein from plants?
Yes, but it might take a little extra work. “Lean meat, low-fat dairy, and eggs have a higher protein density, making an omnivorous diet ideal when targeting protein needs,” says Heather J. Leidy, an associate professor of pediatrics at the University of Texas at Austin and member of the 2020 Dietary Guidelines Advisory Committee. “It’s extremely difficult to meet the dietary reference intakes for protein when eating plant-based protein only with no supplements.”
That doesn’t mean it can’t be done. The key to getting enough protein when following a plant-based diet is to eat a wide variety of protein-rich foods. “While meat may be a more concentrated source of protein, it doesn’t mean there aren’t plant-based foods that are also protein rich,” says Angela Wortley, RDN, a nutritionist and certified intuitive eating counselor in Ann Arbor, Michigan. “The word is slowly spreading that foods such as tofu, lentils, and seitan are also great sources of protein and consuming them has health benefits.”
What makes plant-based protein so healthy?
“The biggest benefit of whole, plant-based protein is that it’s coupled with a blend of healthy fats and fibre,” says Wesley McWhorter, RDN, a spokesperson for the Academy of Nutrition and Dietetics. At the same time, it’s low in saturated fat and has zero cholesterol. This type of eating pattern has been linked to a lower risk of heart disease, type 2 diabetes, dementia, overweight, and obesity.
It’s so powerful that a 2020 meta-analysis of 32 studies in the British Medical Journal found that for every additional 3 percent of calories a person consumed from plant protein, their risk of early death decreased by 5 percent. Compare that to animal protein. Depending on the food, it can be high in saturated fat. And it’s been linked to high cholesterol and heart disease.
Of course, just because a food is rich in plant protein doesn’t automatically mean it’s better for you. “There are also plenty of processed plant-based foods that lack fibre and contain excessive sugar, sodium, and unhealthy fats,” says McWhorter. That’s why it’s extra important to read the nutrition label and ingredient list and to stick with minimally processed sources whenever possible.
(Related: How Does This Trendy Plant-Based Egg Compare to the Real Thing?)
Risks and side effects of plant-based protein
Fibre-rich plant proteins like beans and lentils can do great things for your health. But they can also cause gas and bloating, especially if you’re not used to eating them on a regular basis, explains Sheth. Ditto for plant-based meats that are often made with pea protein.
The good news is you can still eat them. The trick is to add them to your diet slowly to give your digestive system time to adjust, she advises. However, if you’re allergic to soy or nuts, you’ll definitely want to avoid these foods.
What are the best sources of plant protein?
If you’d like to add more plant-based protein to your diet but aren’t sure where to start, try these foods:
- Soy milk: Soy’s complete protein makes soy milk a great plant-based alternative to cow’s milk. For comparable nutrition, look for brands fortified with calcium and vitamin D (and vitamin B12, if you’re a vegan).
- Quinoa: This high-fibre grain (it has 5 grams per cooked cup) also has a low glycemic index, making it a win for blood sugar control. Plus, it contains all the essential amino acids your body needs.
- Tofu: Made from solidified soy milk, tofu is perfect for smoothies, stir fries, and sandwiches. Some brands offer as much calcium as a glass of cow’s milk, so check out the nutrition label.
- Tempeh: This fermented soybean cake is packed with iron, and it’s a good source of zinc. Use it for veggie burgers, or crumble it into tacos or pasta sauce.
- Seitan: Made from wheat gluten, seitan’s meaty texture makes it a smart replacement for meat (unless, of course, you have celiac disease or a gluten intolerance). Try it pan fried or grilled.
- Sorghum: In addition to protein, you’ll net iron, magnesium, and B vitamins from this grain. Serve it as a side dish or pop it like popcorn for a snack.
- Amaranth: This gluten-free grain is also full of inflammation-fighting antioxidants. Try it as a higher-protein alternative to oatmeal.
- Pulses: Along with plenty of protein (roughly 15 grams per cup), these little guys are loaded with soluble fibre and potassium for heart health.
- Bean-based pasta: Whether it’s made from chickpeas, lentils, edamame, or black beans, these noodles are a genius way to give your pasta bowl a protein boost.
- Sprouted grain bread: Made from a mix of beans and high-protein grains, each slice packs 5 grams of plant protein and 3 grams of fibre.
- Nuts: Thanks to a trifecta of plant protein, fibre, and healthy fats, nuts are practically guaranteed to keep you full between meals.
- Plant-based protein powder: If you’re finding it difficult to get enough protein from plants, “either soy or pea protein isolates are a great way to meet protein needs,” says Leidy.
Next: 6 High-Protein Plant-Based Meals This Nutritionist Loves

From the first phone call with my doctor, I knew there’d be obstacles ahead. Seconds after picking up, he started asking questions about my transition that made me uneasy. Right away, he brought up gender-affirming surgery—he wanted to know when I planned to get vaginoplasty.
I knew what he wanted to hear: that I wanted the surgery as soon as possible. The truth was, I didn’t want it at all. I’m non-binary and the way I experience gender is that the concepts of “man” and “woman” exist on opposite ends of a sliding scale. I needed transition care, which for me meant hormone replacement therapy, but not that particular surgery. The immediate focus on genitalia made me uncomfortable. I was just starting to transition and wasn’t thinking about surgery.
Many doctors—even trans specialists—expect patients to accept the care most commonly associated with a male-to-female or female-to-male medical transition, which is hormone therapy leading toward either vaginoplasty or mastectomy. I swallowed my pride and told the doctor that I wanted vaginoplasty, even though I didn’t. His tone shifted right away. When I agreed, at least in theory, to treatment that adhered to the gender binary, he seemed to understand the path forward for me under his care. It was demoralizing, but I was one step closer to the care I deserve and the medications that would change my life, which for me were testosterone blockers and estrogen.
Sadly, my experience isn’t unusual. According to The Canadian Journal of Human Sexuality, there is an overemphasis on stereotypical gender norms within trans health care. In my experience, many medical professionals assume that if you don’t conform to male identity, you must be female—or vice versa. The medical model of transitioning is grounded in the gender binary, which creates problems for non-binary patients like me, who, as the study notes, commonly have to prove they’re “trans enough.” Making matters worse, studies have found that medical professionals don’t receive education about trans health care. In a poll published in the Canadian Medical Education Journal, 71 percent of family doctors said trans care was within their purview, but just 10 percent felt prepared to provide it.
Making my way through the health care system as a non-binary person has felt like taking a series of tests where a “wrong” answer could halt my care. When it comes to trans health care, there are long wait times just to get in the door and patients commonly face systemic transphobia within the medical care system. Doctors and other health care providers wield great power over trans patients, too. I felt like my care could be rescinded without warning. So in that moment, on the phone with my doctor, I realized that being transgender means becoming your own health care advocate. Armed with research and self-knowledge, I’ve stood up for myself and demanded to transition on my own terms. These are the lessons I’ve learned.
Finding a trans-affirming doctor is the first test
Finding a doctor is exceptionally difficult for trans folks. Queer community centres or associations are a good place to start—they often offer resources for trans folks looking for medical care. You can also try Googling “queer non-profit” or reaching out to a local Pride or PFLAG group. In Ontario, for example, I recommend 2SLGBTQ+ organizations like The 519 or AIDS Committee of Toronto. They often offer resources for trans folks looking for medical care, though they can be harder to find in smaller cities or towns.
In Toronto, I saw a wonderful queer doctor at a queer clinic. He connected me to a counsellor who was the first person I spoke to about transitioning. “If you are trans,” she asked me, “would you transition?” The question showed me she had an open mind and knew that not every trans person wants to medically transition. At every turn, she put me in the driver’s seat; there was no pushing of any particular narrative about the “right” way to transition.
When I moved to Montreal a few years back, I received a list of trans-friendly doctors from Action Santé Travesti(e)s et Transsexuel(le)s du Québec. I spent a month calling every name on the list only to discover that the average wait was two years just for an appointment. When I finally landed an interview with the man who is now my doctor, I knew he wasn’t the right fit, but I was tired of waiting. I needed care.
Your gender will be tested against stereotypical norms
The next test came when you’ve decided on your transition trajectory. In my experience, doctors expect you to reaffirm their version of what a transition should look like.
When I started seeing my doctor in Montreal, he pushed back on nearly everything, from the medications I wanted to my surgery choices. But things improved drastically when I started to conform to his notions of femininity. Before appointments I would shave my arms and legs, then put on mascara, blush and a padded bra. It was performative, but it felt like my only route to care. (A 2021 Canadian study revealed that physical appearance, including gender expression, plays a factor in whether trans patients are given access to transition-related care.)
Having to “prove” my femininity really hurt. At that moment, I had to remind myself that it didn’t mean that my journey or how I want to transition isn’t valid, it was just something I had to do to get through.
Even if you pass a test, your doctor’s advice can be harmful
My doctor’s neglect in understanding what my body means to me as a non-binary person has even led to harm. When I was finally prescribed a testosterone blocker, he failed to mention the impact it would have on my penis. On blockers, blood flow to your penis is stunted and if you don’t exercise the muscles, such as with masturbation, you can lose the ability to have an erection.
After a physically painful experience, I did my own research and found out what was going on. I also found a solution: a low dose of Cialis. When I suggested it to my doctor, he immediately brought up vaginoplasty again in a way that I felt questioned my transness. He assumed that because I was in the process of transitioning, I wouldn’t want a functioning penis. His notion of transness was wrapped up in sex rather than gender and didn’t allow room for me to have a healthy non-binary body on my own terms.
I dug in my heels. No one was going to tell me that my body functioning healthily was incompatible with my transition. Eventually he relented, but I had to fight for myself.
When the system fails you, you have to take care of yourself
Through all these tests, there’s one thing I’ve learned: I have to take care of myself. My doctor wasn’t providing the care I needed, so I had to learn to take care of my body—and love it—myself.
For me, that meant putting my lifelong love of exercise in a context that aligned with my gender. I’ve never felt more affirmed than when I put on athletic wear and a sports bra for a run.
Depression and anxiety often go hand in hand with transitioning, so my advice is to start small and, slowly, you’ll find what’s right for you. Remember: even if the best health support you receive comes from within, you’re worthy of that care.
*Name has been changed to protect the identity of the author.
Next: ‘We’re Not Doing a Good Enough Job’: How Canada’s Health Gap Is Affecting Women
When psychologist Dr. Lori Brotto published Better Sex Through Mindfulness in 2018, she was deluged with requests from readers who wanted to be treated by her or to participate in sessions at her Sexual Health Research Lab at the University of British Columbia. Unable to meet all of these requests, Brotto instead published a companion book, The Better Sex Through Mindfulness Workbook: A Guide to Cultivating Desire. It includes exercises to help women understand their emotional and physical connection to their sexual selves. Here, Brotto talks about why, contrary to popular belief, hot sex might require a little bit of work.
What is the connection between mindfulness and better sex?
The connection is strong. In order to understand why it works, we need to take a step back and understand what the main contributors are to sexual problems. We know that distraction, judgment, irrational thoughts, preoccupations, catastrophizing, spectatoring, all of these concepts have been shown to contribute to sexual difficulties, especially low desire. And mindfulness, which really boils down to present-moment, non-judgmental awareness, is quite a simple set of skills that addresses every single one of those potential barriers that impede sexual desire. In our science, we’ve evaluated that. We’ve been able to demonstrate not only that mindfulness works, but that the improvements people see are lasting. A year later, people are still practicing the skills and still benefiting from them.
There is this pervasive myth that sex needs to be spontaneous and thrilling and, like, “rip your clothes off” all the time. But your research shows that good sex takes effort. How do we let people know that effort is sexy as well?
I often say, “Think about anything that’s meaningful and important to you, that was not planned. There are probably very few wonderful events that were totally spontaneous.” People can easily relate to that. They’re like, “Yeah, I planned that dinner party, I planned that vacation.” You can also plan foreplay, you can plan the fantasies that you’re having while leading up to the sexual encounter, so that you’re not kind of jumping into the cold water fully dressed. You’re slowly kindling the fire by eliciting some erotic scenes in your mind. We really want to normalize planning, but also talk about it in a very pro-sexy way as well.
You acknowledge that some people may be skeptical about the concept of mindfulness, and that’s quite all right. How do you allay those concerns?
I’ll give you an example. We started running our mindfulness groups for women with vulvo-vaginal pain—one in five women have chronic burning, stinging sensations with any kind of vaginal penetration. When we first started introducing mindfulness to that group—because there’s a whole literature on mindfulness for pain—the women were really skeptical. It’s because they had been led to believe that there was some injury, there was some irritation or infection at the vulva and vagina that was causing their pain. It makes sense that they would think this, because their doctors would dismiss them. We presented them with actual scientific studies that showed that, number one, all chronic pains are maintained in the brain, and, number two, that mindfulness changes the brain. If we can change the brain and change the pain centres of the brain, it should have this downstream effect of improving vulvar pain as well. The way we address the skepticism is science.
We live in such an incredibly stressful world right now. How do you convince women that it’s okay for them to take time every day to do their mindfulness practice?
I’m going to sound like a broken record, but it really comes back to the science. Originally, when mindfulness was being evaluated back in the late 1970s and early 1980s, it was always in the context of these comprehensive, eight-week practices, at least an hour a day, or seven hours of walking mindfully through a forest. There’s been a lot more research since then, showing that even 10 minutes a day can produce structural and functional changes in the brain that allow us to really benefit from mindfulness. We know that multitasking actually leads us to be less efficient. It leads us to take less pleasure in the things that we’re doing and make more mistakes. By investing a short amount of time in mindfulness, we’re actually saving time in other areas of our day.
We’ve all just come through two years of Zoom fatigue and trying to get our kids through school. What effect has the pandemic had on people’s libidos?
Some of the early speculation in April 2020 was that we’d see a baby boom. Because, of course, no one had anything else to do but stay home and have sex with their partners. We had all this extra time on our hands. When we studied it, and we followed people over time, we found the opposite. Every other study found the opposite as well. Desire went down, sexual activity went down. The only thing that went up was masturbation. Probably it was a coping mechanism, a way to feel some brief moments of pleasure in an otherwise dismal life stage.
Do you get the sense that everybody feels like other people are having more and better sex than they are?
It’s more than a sense, because I have patients tell me that constantly. They think they’re the only one that struggles with this. I’ll say, “Have you really asked other people?” And they’ll say, “No, I haven’t asked. But I can tell by looking at them, the way they hold hands, they’re having tons of sex.”
We tend to think that desire must come first, and arousal will follow. But you challenge that thinking. How are arousal and desire related?
We know from scientific studies that the direction of arousal first and then desire is far more common than we previously thought. It’s far more common in longer-term relationships, where we might agree to sexual activity for non-sexual reasons. It’s our anniversary, or I want to feel close, I want to say thank you, I want to get rid of my headache, what have you. In the encounters, as long as the kinds of stimulation and exchanges are right for her, and right in a way that elicits her arousal if she continues to focus and stay present, that can give way to a wanting. She probably feels the wanting well into the encounter, even if she doesn’t feel it at the outset. That message, that kind of normalization of feeling neutral at the outset, is really important because so many women feel broken when they don’t feel horny.
You write that one-third of women struggle with low or declining desire. Is this low desire a problem for everyone who experiences it?
No, it’s not. That’s a really important question. If you’re going through a stressful period you might say, I’m not interested in sex. I’m recovering from surgery, or I’m tending to an ill partner, or I have a major stressful life event happening. It’s a smaller proportion of those with low desire who experience distress. And even in distress, we need to be careful because sometimes it’s the partner’s distress. To qualify for a disorder, one needs to have the symptom of low desire, combined with clinically significant personal distress.
Part of mindfulness is an acceptance of all emotions, whether positive or negative. Tell us about the metaphor of the guest house, which you use to explain this process.
Women have a really hard time admitting that they feel anger—like there’s something really wrong with us if we if we feel angry or irritable or irritated. The mindfulness approach shows that our effort to get rid of anger and emotions like that creates a lot of suffering that then harms us. “The Guest House” is a translated poem by the Persian poet Rumi. It talks about inviting all the guests, because some of them might be clearing you out for some future delight. It’s in the acceptance of emotions that suffering starts to fade.
There are lots of myths out there regarding menopause and sex. What are some of those myths?
That sex ends with menopause. That menopause depletes you of all your hormones, which it doesn’t—during the up to 10 years of perimenopause, there are actually fluctuating levels of estrogen. That aging women can’t initiate sex. That if you don’t have a partner, you’re asexual. That young people are sexually promiscuous and have no sexual problems. I could go on and on.
Why is good sex important for mental and physical health?
The World Health Organization has declared that sexual health is a component of quality of life. Now, if you’re an asexual person, this is not going to be relevant, because asexual people just don’t have sexual interest at all and are totally fine with it. Removing asexuals from that group, sexual health can directly contribute to self esteem, to physical health, to relationship satisfaction. All of that has been supported by a lot of science. When sexual health is not going well, it can also directly contribute to relationship conflict, depression, anxiety, and stress. Sexual health and general health and quality of life are tightly intertwined.
Next: What Exactly Is Tantric Sex, and Should I Try It with My Partner?
My mom says my grandpa’s napa cabbage salad was so famous that people would specifically request it whenever he was invited to a get-together or had friends over for dinner. It couldn’t be simpler: you salt napa cabbage, squeeze out the water, and toss the juicy shreds with slippery vermicelli noodles and a sesame oil vinaigrette zingy with garlic and cilantro. It’s sort of like a Chinese slaw—fresh with a snap of acidity, cleansing for the palate, and fantastic cold. Start the recipe in advance to allow the flavors to be absorbed and develop as it sits. I often prepare one big batch to have at lunch during the week— with its sweet, sharp juices, it’s great paired with a steamed or roasted sweet potato.
Napa Cabbage & Vermicelli Salad
Báicài bàn fěnsī
白菜拌粉絲
Serves: 6
Ingredients
- ½ medium head (1 pound / 450 grams) napa cabbage
- 1 small Persian cucumber, thinly julienned
- 1 teaspoon kosher salt, plus more to taste
- 2 ounces (56 grams) mung bean vermicelli noodles, soaked in warm water for 10 minutes
- ½ medium carrot, finely julienned
- 1 scallion, both white and green parts, cut into 3-inch segments and thinly julienned
- 4 garlic cloves, finely chopped 3 tablespoons soy sauce
- 3 tablespoons pale rice vinegar 2 tablespoons sugar
- ½ teaspoon MSG
- 2 tablespoons toasted sesame oil
- ½ cup coarsely chopped fresh cilantro
Directions
Separate the cabbage into leaves. Lay out one leaf and slice it horizontally through the white stem portion to make it thinner. Repeat with the remaining leaves, then stack and cut them crosswise into ¹⁄₈-inch shreds. Place in a colander with the cucumber and toss with the salt.
Meanwhile, bring a large pot of water to a boil. Add the vermicelli and cook according to the package instructions. Rinse under cold water and drain. Snip with kitchen scissors into shorter, more manageable lengths.
Squeeze out the excess liquid from the cabbage and cucumber by pressing them between your hands. Drop each squeezed handful into a large bowl without rinsing it. Add the vermicelli noodles, carrot, scallion, garlic, soy sauce, vinegar, sugar, MSG, and sesame oil and stir well. Taste and adjust the salt and other seasonings as needed. You can enjoy this immediately or chill it in the refrigerator, covered, for a few hours to let flavors meld. Stir in the cilantro just before serving for the freshest flavor.
Excerpted from The Vegan Chinese Kitchen by Hannah Che. Copyright © 2022 Hannah Che. Photographs by Hannah Che. Published by Appetite by Random House®, a division of Penguin Random House Canada Limited. Reproduced by arrangement with the Publisher. All rights reserved.
Next: This Coconut Clay Pot Taro & Edamame Is the Vegan Dish You Need This Season
Noticing more hair in your brush or drain, or seeing your scalp starting to peek through your ’do? You’re not alone—about 40 percent of women experience hair loss by age 50. But don’t sound the alarm just yet: There are lots of explanations behind hair loss. It might be a response to a new medication, to stress (likely courtesy of the pandemic), to giving birth or even just to a change in the season. But we can also point the finger at genetics and certain health conditions, such as a thyroid disorder or a sex-hormone imbalance.
If the problem doesn’t resolve after a few months and it’s bothersome, you may want to consider interventions. Luckily, dermatologists have a few treatment options that range from easy-to-apply topicals to more invasive procedures.
If the hair loss is caused by inflammation, including cicatricial (scarring) alopecia, a topical cortisone cream and injections into the scalp can help stimulate hair growth, says Dr. Heather Woolery-Lloyd, a Miami-based dermatologist and faculty member of Canada’s Skin Spectrum Summit.
Non-inflammatory hair loss includes androgenetic alopecia and female pattern baldness, which “generally starts at the top of the head as well as the frontal areas,” says Dr. Marlene Dytoc, an Edmonton-based dermatologist. It can be treated with topical minoxidil, also known as Rogaine, “which has been proven to retain hair and sometimes grow new hair,” says Woolery-Lloyd. The topical version is available over-the-counter and the oral medication by prescription.
Depending on the cause of hair loss, dermatologists also recommend platelet-rich plasma (PRP) therapy, in which your own blood is injected into your scalp to stimulate hair growth. Another option is low-level light therapy that’s emitted from a helmet you can wear at home, which has been shown to boost hair density.
So what about all those shampoos and conditioners on the market that promise to make your hair grow? “If my patient wants to use them because they think it works, I have no problem with that,” says Woolery-Lloyd. But she won’t recommend these products unless the ingredients have been scientifically proven to work.
The best thing you can do to address hair loss is talk to your dermatologist. As Woolery-Lloyd says, “If we catch it early, treatment options are better.”
Next: The Best Skin Care Routine for Your Age, According to Dermatologists
Like many things in the past two and a half years, Pap tests were put on hold to limit close contact. And we can’t say we missed them—hopping into the stirrups and bracing for the cold speculum is no one’s idea of a good time. But just how necessary are they?
Pap smears screen for cervical cancer by detecting abnormal cells in the cervix. Typically, abnormal cervical cells are caused by a human papillomavirus (HPV) infection, and often resolve on their own. If they don’t, these abnormal cells need to be treated or they could cause cervical cancer (1 in 168 women are expected to develop the disease in their lifetime—but it is highly treatable when detected early). Since it takes about five years or longer for abnormal cells to potentially cause cervical cancer, Health Canada changed its recommendation for screenings from every two years to every three years. But, even with this increased time frame, regular screenings are still not feasible for many women. Work obligations, child care burdens, financial restraints, and now pandemics—not to mention embarrassment and fear—are among the many barriers preventing women from getting their Pap tests. Could there be a better way to screen for cervical cancer?
Dr. Gina Ogilvie, affiliate scientist for BC Cancer and one of Canada’s leading experts on HPV, is answering that question with a resounding yes. It’s actually possible to administer a test yourself, in the convenience of your own home, and get accurate results—and some women in B.C. are already doing just that.
Earlier this year, BC Cancer launched an at-home cervix screening pilot project to test what happens when screenings are made more accessible. The agency is targeting a mix of remote and urban areas of the province where there are many people who have never been screened or are overdue for screening. Participants are mailed a self-collection kit that includes a swab and a container (no cold, daunting metal speculum in sight). Then, participants mail their sample to a lab, where technicians determine whether the cells are infected with the specific high-risk strains of HPV that can cause cervical cancer.
We chatted with Ogilvie to learn more about the pilot and how it might help women across the country.
(Related: Questions You Should Ask Your Gynecologist)
Why is it important to test for cervical cancer every three years, and not more often?
A Pap test is a screening—meaning it’s done when there are no symptoms present. We use it to look for changes in the cells that could potentially lead to cancer. The fortunate thing about cervical cancer is that it’s a very slow-growing condition. So we have to balance finding precancerous lesions while not over-calling benign lesions that may look a little funny but that, if we gave them time, would actually resolve. What we’ve found over the years is that by extending the interval from two years to three, we reduce the rate of false positives, so we don’t send women for unnecessary follow-up procedures.
Why can the cervix screening in your pilot be done at home but a Pap smear can’t?
With the Pap, women have to undergo a pelvic examination so the practitioner can see the cervix to get the cells. In contrast, the HPV test can be collected by women themselves because the sample does not have to come from a specific part of their anatomy, but rather from vaginal secretions.
How else does cervix screening differ from a Pap test?
Unlike Pap tests, cervix screenings check for HPV specifically. Like pap tests, HPV testing is recommended every three years. But we’ll soon be able to extend that interval to five years because the HPV test is even better than Pap tests at detecting the potential of developing precancerous and cancerous lesions. When someone has a negative HPV test, we can be confident that, in the next five years, it’s very unlikely they will develop any precancerous lesions. We have very good evidence that, even with the extended screening interval, HPV testing performed better than Pap smears, thereby limiting iatrogenesis illness, which is an illness caused by the health system.
How do women conduct the test themselves, exactly?
It’s like putting in a tampon—insert the cotton swab, twirl it around, get secretion on it, take it out, put it in a container, mail it in, and it’s examined by a lab.
Are there any risks involved with an at-home cervix screening? Is it possible to do it incorrectly?
Women can do this very safely, they can do very accurately. It’s also been rolled out in places like Australia and Wales, so we have even more proof that it works.
What happens if the test comes back positive?
We’re doing this screening to get women who are positive into treatment. If someone’s positive, they would go for a follow-up Pap smear, because that helps us understand whether the HPV has progressed. Alternatively, if they have a certain HPV, like types 16 or 18, they would go right to treatment because we know those HPV infections are very likely to progress to precancerous lesions. Treatment for those would include a colposcopy exam, where a practitioner examines the cervix, looks to see if there’s anything concerning, and, if there is, they remove that tissue.
Would a Pap smear ever be preferred over an at-home cervix screening?
Some folks will choose to go to a practitioner because they want a full genital examination. Or maybe they see something they’re worried about—lesions, bleeding, abnormal discharge. For anything like that, you should always see a practitioner.
A common misconception is that Pap smears also test for ovarian cancer and sexually transmitted infections. Is there concern that, by limiting the need for women to visit their doctor, cases are being missed?
All the important things that happen during a practitioner exam—say, STI testing or reminder about mammograms—still need to happen. You still need your check-ups, and if you’re sexually active, you still need your STI screenings.
Is there a timeline for when the at-home test will be the standard for cervical cancer screening and available across Canada?
We’re first committed to spreading information so people understand this can be done safely and effectively. In B.C., we’re going to continue to expand and offer it and then summarize the data. Then, hopefully, we can use that to inform our provincial policy and to urge other provinces to move forward.
This interview has been edited and condensed for clarity.
Next: This Canadian Company Made Pregnancy and Ovulation Tests So Much Better