For years I thought of beef curry as a dish that required simmering chunks of stew beef for hours until tender. But for a weeknight, I wondered if there was a way to do it quickly and without a pressure cooker. Then I remembered my days working at a quick-service Thai restaurant, where we churned out pots of fork-tender beef curry in 45 minutes. The secret was using thinly sliced beef and choosing a flavorful but not-too-tough cut so it would not take a long time to tenderize. The restaurant used flank, which was great but a little lean for my liking. I found chuck top blade to be the perfect choice in terms of flavor and fat content, and it only takes about 20 minutes of simmering to become fork-tender.
Quick Yellow Curry with Beef
Gaeng Garee Neua | แกงกะหรี่เนื้อ
Serves 4
Cooking Time: 45 minutes
Ingredients
Yellow curry paste
- 0.7 ounce (20 g) mild dried red chilies, cut in ½-inch (1.2 cm) chunks
- 1 tablespoon (15 ml) coriander seeds, toasted 1½ teaspoons (7 ml) cumin seeds, toasted
- ½ teaspoon (2 ml) white peppercorns 1 teaspoon (5 ml) table salt
- 1 stalk lemongrass, bottom half only, finely sliced
- 2 tablespoons (15 g) chopped ginger
- 2 tablespoons (15 g) chopped galangal
- 1 tablespoon (8 g) chopped turmeric, or ½ teaspoon (2 ml) ground turmeric
- 6 cloves (30 g) garlic, chopped
- ½ cup (70 g) chopped shallots
- 1 tablespoon (15 ml) curry powder
- 2 teaspoons (10 ml) fermented shrimp paste (optional)
Curry and beef
- 1½ pounds (675 g) chuck top blade steak (see note)
- 1 teaspoon (5 ml) table salt
- 5 to 6 tablespoons (75 to 90 ml) yellow curry paste, store-bought or homemade, divided
- 2 cups (500 ml) coconut milk, divided
- 1½ tablespoons (18 g) finely chopped palm sugar, packed
- 1 to 2 tablespoons (15 to 30 ml) fish sauce 1 tablespoon (15 ml) tamarind paste, store-bought (optional)
- 10.5 ounces (300 g) waxy potatoes, such as new or red-skinned potatoes, cut into 1½-inch chunks
- ½ medium (120 g) yellow onion, julienned
- ¾ cup (100 g) halved cherry tomatoes Jasmine rice, for serving
Directions
For the curry paste
Using a coffee grinder, grind the dried chilies, coriander seeds, cumin seeds, peppercorns, and salt into a fine powder.
If using a heavy-duty mortar and pestle, add the lemongrass, ginger, galangal, and fresh turmeric, and pound into a fine paste. Add the garlic and shallots, and pound into a fine paste. Add the ground chili mixture and pound until well combined. Add the curry powder, ground turmeric, and shrimp paste; pound to mix.
If using an immersion blender, place the lemongrass, ginger, galangal, and turmeric in a narrow container, such as a glass measuring cup.
Then top it off with the garlic, shallots, and shrimp paste (it is easier to blend with the moister ingredients on top). Use the immersion blender to blend everything until fine. You will need to lift and reposition the blender several times, stopping to scrape the bottom and bringing it to the top halfway through. Once the mixture is fine, add the ground chili mixture, curry powder, and ground turmeric, and blend to mix.
Use right away, store in the fridge for up to 3 days, or divide into two portions and freeze for up to a few months.
For the curry with beef
Slice the steak into 1/8-inch (3 mm) pieces, removing any silver skin on the exterior (the little strip of connective tissue running through the middle of the steak is fine to leave).
Place the beef in a medium pot and add just enough water to sub- merge it. Add the salt and 1 tablespoon (15 ml) curry paste and stir to mix; bring to a simmer over high heat. Turn the heat down to low and simmer for 20 to 25 minutes, until fork-tender. The timing will vary if you use a different cut of meat. Skim off any scum that floats to the top.
While the beef cooks, make the curry sauce. In a medium pot, bring ¾ cup (185 ml) coconut milk to a boil over medium-high heat, then add the remaining curry paste and stir to mix well. Turn the heat down to medium and stir frequently until the mixture is very thick and the coconut oil separates from the paste, about 5 minutes (the oil may not separate depending on the coconut milk you’re using; this is okay).
Add the remaining coconut milk, sugar, 1 tablespoon (15 ml) fish sauce, and the tamarind paste to the curry. Stir to mix, then bring to a boil over medium-high heat.
Add the potatoes and onions, and simmer for 5 minutes, then remove from the heat while you wait for the beef to be done; the potatoes should not be fully cooked at this point.
Once the beef is tender, use a slotted spoon to transfer only the beef into the curry. Then add only as much of the beef cooking liquid as needed to keep everything barely submerged. Taste the sauce and adjust the seasoning with more fish sauce, tamarind, or sugar as needed.
Turn the heat to medium and simmer the curry for another 5 to 10 minutes, until the potatoes are fully cooked.
Stir in the tomatoes, turn off the heat, and allow the tomatoes to soften in the residual heat for 1 to 2 minutes. Serve with jasmine rice.
Cooking Beef Out of the Curry: Why not just simmer the beef in the curry itself, you ask? The technique used in this recipe is one that’s commonly used in Thai cuisine when cooking with beef, for a couple of reasons. When you simmer the beef, you will notice a lot of brown scum in and on top of the liquid, which would discolor the otherwise beautiful curry sauce. As well, many Thai people don’t like the strong beef flavor that would be in the curry if it were all cooked together, especially because beef in Thailand can be quite gamey. And, in our weeknight-friendly case, it also saves time so that we can make the rest of the sauce while the beef is doing its thing.
Do-ahead: The whole curry can be made up to 3 days in advance and reheated. If reheating, be sure to not overcook the potatoes—or add them when serving.
Notes: If you can’t find chuck top blade, you can choose other cuts of beef that are flavorful but not too tough. Most inexpensive steaks sold for marinating and grilling fit this bill, and if possible, choose one that is not too lean. If you have time to cook, you can choose any stewing beef and increase the cooking time accordingly.
If you don’t have tamarind paste, no need to buy or make it just for this recipe. We just need a little bit of acid to brighten up the sauce, so a few dashes of Worcestershire sauce or a squeeze of lime at the end will also do.
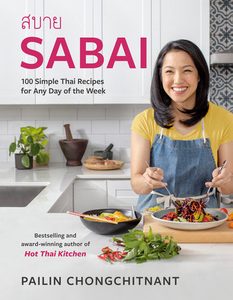
Excerpted from Sabai by Pailin Chongchitnant. Copyright © 2023 Pailin Chongchitnant. Photographs by Janis Nicolay. Published by Appetite by Random House®, a division of Penguin Random House Canada Limited. Reproduced by arrangement with the Publisher. All rights reserved.
Next: A Simple Recipe for Old-School Pad Gaprao
Every year, more than 100,000 Canadians have a stroke, and around half of them are women.
Most stroke sufferers will experience what’s called an ischemic stroke, where a clot blocks blood flow to a part of the brain. When the cells on the other side of that clot stop getting oxygen and nutrients, they die, which causes brain damage and lasting symptoms like memory loss or paralysis. Because each side of the brain controls the opposite side of the body, people who have a stroke in the right side of their brain will often be paralyzed on their left side (and vice versa).
Others will have a hemorrhagic stroke, which happens when a weakened blood vessel in the brain leaks or bursts, flooding the surrounding area with blood and causing the cells there to die.
Finally, a mini-stroke (the medical term is a transient ischemic attack, or TIA) is when a clot temporarily blocks blood flow to the brain before breaking up on its own. It causes symptoms for an average of 15 minutes and resolves within 24 hours, with minor damage. But it’s often a “warning shot” that you’ll have another stroke within the next few days, says Michael Hill, a neurologist at the University of Calgary and Foothills Hospital and a prominent stroke researcher. For that reason, it definitely warrants an ER trip.
The most important thing to know, says Hill, is that “the main risk factors for stroke are one: hypertension, two: hypertension and three: hypertension.”
He explains that blood clots usually develop from uncontrolled high blood pressure—also known as hypertension—combined with additional factors (such as high cholesterol or smoking). When the pressure of the blood flowing within your arteries is higher than it should be, it damages the walls of those arteries, and your body dispatches white blood cells to the site. When that damage is combined with high cholesterol floating by, sticking to the white blood cells, it results in the accumulation of plaque on the artery wall. The plaque may cause clots, and a big clot can completely block the artery it’s in, or float to another part of your body and cause trouble there. If it blocks the blood flow to your heart, that’s a heart attack. If it impedes the blood flow to your brain, that’s a stroke.
This is why it’s so important to check your blood pressure periodically. Both women and men should aim for a reading under about 120/80 mm Hg.
The risk of stroke is also higher if you are older than 55; if you have a family history of stroke; if you are obese; or if you have diabetes, high blood cholesterol or atrial fibrillation. People living in poverty (who are more likely to be women than men), some members of racialized communities and Indigenous people, and people living in rural or remote areas are also more likely to have risk factors for stroke, and are less likely to have access to consistent or comprehensive management of those health issues.
Recently, newer research has revealed heightened stroke risks that are specific to women: Having endometriosis, taking estrogen-containing birth control, being pregnant and being on hormone replacement therapy all slightly increase the likelihood of stroke. If you experienced pre-eclampsia during a pregnancy, your risk of a stroke later in life doubles.
But while some of those risk factors might be out of our control, there is plenty that women can do to lower their risk of stroke, including quitting smoking, getting active, eating more fruit and vegetables and keeping blood pressure in check.
Some good news: Over the past decade, medications and treatments for strokes have improved dramatically, and considerably more Canadians who suffer a stroke now survive. One newer, game-changing treatment is called endovascular thrombectomy (EVT), in which doctors go into the bloodstream after the clot has blocked the blood flow with a small flexible tube and physically pull the clot out. At Foothills, which was one of the first hospitals to test and pioneer this extraction procedure, Hill worked on a study finding that, for very large, serious strokes, EVT has radically improved patient quality of life and cut death rates in half.
“It has transformed care for that group of people,” says Patrice Lindsay, director of health systems at the Heart and Stroke Foundation of Canada.
But these new meds and interventions work best if people seek help within minutes of having a stroke. “Statistically, we can show that every 10 minutes makes a difference,” says Hill. “Coming in early can make the difference between walking out of the hospital two days later or being in long-term care, paralyzed.”

Carla Hindman
Communications professional and 44-year-old mother of three in Toronto
I was only 41 when I had a stroke. I was at my office, and at around 1 p.m. I went to the bathroom. When I went to wash my hands, I looked at myself in the mirror and I couldn’t see properly. I thought, This is really weird. When I finished washing my hands and walked back to my desk, I put my head down and started to cry. A colleague beside me was like, “What’s going on?” And I said, “Something’s wrong with my eyes.” But then I said, “I think I’m having an ocular migraine”—I had had one before. I didn’t know that vision changes were also a sign of stroke.
My colleagues decided to call my husband, Matt, who worked across the street. We jumped in a cab together to go to our doctor’s office, and by the time we got there, my face was drooping, I was slurring and I had weakness in my left side. Matt was thinking, Oh my God, this looks like a stroke. Since we were in front of my family doctor’s office, he decided to take me inside instead of wasting more time going all the way back downtown to the ER—he thought it would be better to get medical advice as soon as possible. But they took one look at me at the doctor’s office and called 911.
When we were waiting for the ambulance, Matt told me to raise my hands. I raised only the right one, and he said, “Both of them!” I yelled back at him, “I am raising both of them!” but my left arm was dead at my side—I just didn’t know it.
I don’t remember anything after that until midnight. But I had left the doctor’s office in an ambulance, and they had assessed me, given me clot-busting medication and put me in the ICU. My mom had flown in from Ottawa to be with me, and Matt had gone home to be with our three kids. The nurses were coming in every once in a while, showing me flashcards, asking me what the pictures were. My mom said that at midnight it was like a switch flipped, and I was back to normal.
At the hospital, they found a hole in my heart, which I had no idea was there. They said that this was what caused the stroke—those holes can allow blood clots to travel to the brain instead of the lungs, where they would normally go. A year later, I had a procedure to repair it, and now my risk of a stroke is as low as an average person’s.
I was extremely, extremely lucky: I didn’t have any lasting physical deficiencies after the stroke. But I do have a few issues with short-term memory still, and sometimes I have trouble coming up with the word I want. And I was exhausted afterward—I was off work for a month and then had to do a staggered re-entry after that.
I didn’t know that people my age could have strokes, but now I have met so many people who have had them in their 40s. It happens all the time. I think everyone should know what the signs of a stroke are and that vision changes are one of them. If more people knew the signs, and that young people can have strokes, they might feel empowered to call 911 in situations like mine, and a lot more people could get the help they need faster.

Kathy Isaac
Cybersecurity executive and 47-year-old married mother of two in Ajax, Ontario
I had a stroke two years ago while I was in the ICU, hospitalized for COVID. After about two days, I woke up with extreme nausea, and I was dizzy and vomiting for days. But my doctors didn’t realize what was happening, even after my left hand started to feel strange and heavy. Eventually, I realized I couldn’t hold my fork in that hand.
A week later, when a physiotherapist came to prepare me to go home, she was the one who noticed the signs of stroke. They did a brain scan, and a doctor came the day before I was supposed to leave and said, “I have bad news—you’ve had a stroke.” I thought he had the wrong person. I actually said to him, “No, I’m Kathy.”
In my head, I’m thinking, I’m 45 years old. Strokes are for older people. I’m better, I’m going home.
Even after I realized something had happened, I still felt like, if I’ve had a stroke, what does that mean? They started to talk to me about neuroplasticity, and they explained that the best window for recovery is the first six months.
So I wasn’t wasting any time. I started walking in my hospital room while I was still attached to oxygen. Then I did outpatient therapy: physical therapy, occupational therapy and a little bit of speech therapy, too. I had a singular goal: I wanted to go in one direction, to make progress. I did everything they asked. And I did well—I hit the physical milestones by about three months out.
But it still all felt so heavy. I had a meltdown one day with my physiotherapist and just cried. Eventually, I was connected to the Heart and Stroke Foundation and the March of Dimes. I was in a young stroke survivors’ group for a long time.
Just before I went into the hospital for COVID, I had graduated from Ivey Business School in London, Ontario, with my MBA. It was hard, really hard—I did it while I was working as an executive, and as a wife and mother. I thought about quitting. But the motto at Ivey was “trust the process.” And I decided, no, I’m gonna tough it out.
That was an important life lesson. When I went to rehab, I knew to just put in the work, and trust the process. I’m a born-again Christian and I do believe, like the Bible says, that all things work together for good. To me, the MBA prepared me.
I’m a few years out from the stroke now. My mobility is really good, and work is going well, too—I think I perform very well. But I have to work every day to not regress—I walk or use my spin bike. And I’m not the same. My balance can be a little wonky, I can’t handle noisy situations and I have more anxiety. I still have precision issues in my left hand because the message from the brain to my left hand is delayed. If I type with both hands, the right hand will be fine and the left hand will be behind.
One of the biggest challenges I’ve had is friends and acquaintances thinking I’m all better. I’m not looking for sympathy, but I need people to understand that I’m not 100 percent. Even when I park in a disabled parking spot—which I need to do—I’ve been confronted by strangers when I get out of my car. Because I don’t use a cane or a walker, I don’t get the understanding and help that I need.

Earle Hoyte
76-year-old retired church administrator, caregiver and grandmother in Toronto
One weekend I went on a short trip. After I got home, off the train, I said something to my granddaughter, and it felt like it wasn’t coming out right. But when I asked her if she could understand what I was saying, she said yes. And I also felt very tired, so I just went to bed.
In the morning, my tongue felt very heavy, and when I went to put on my lipstick, my hand kept falling down. My son-in-law and daughter-in-law were there and they said, “You don’t sound well—we should take you to the hospital.” I knew I wasn’t fine; I felt different. But I didn’t know it was a stroke. I thought only old people had strokes and I was only 75.
And I didn’t realize what else was happening to me. At the hospital, the nurses recognized it immediately as stroke and pushed me through. The doctors did a lot of tests. But I didn’t realize the effect the stroke had on me until the doctor asked me to sign my name on a document. It was only then that I realized I couldn’t. I was just scribbling.
They told me my stroke was caused by atrial fibrillation—an irregular heartbeat. I didn’t know I had it before the stroke. They put me on blood thinners, and with atrial fibrillation, it’s quite easy to have another stroke. So I have to be quite careful, and take my tablets every day.
After I left the hospital, I was referred to the University Centre location of Toronto Rehab. Before I went, I didn’t know what to expect. I was scared. But everybody I met there was so warm to me—even the receptionist. They were very positive, and it helped very much.
I went there for three months, as an outpatient. We worked on the physical: I had to walk with a walker, and up and down stairs, and practice stepping over things. They focused on my balance a lot, too.
They also worked on my memory, because whenever I tried to speak, I had to think for a long time to remember what I wanted to say. And a speech therapist helped with my voice—I used to sing in the church choir, and I couldn’t sing anymore. My driver’s licence was suspended, and they worked on that with me. I even did a driving simulation at Toronto Rehab.
At one point, I didn’t want to go, because I was feeling depressed. They referred me to a social worker, and to the March of Dimes program for people with disabilities. Now I go several times a week. March of Dimes has a stroke textbook, too, that I wish I had had before, because it tells you what to expect, what questions to ask, who is going to see you and what each person will do for you.
I’ve improved a lot—I’m back to singing in the choir, and I’m able to be a caregiver to my elderly sister. But there are things I can’t do anymore, like baking or reaching items off the highest shelves. I had to completely rearrange my kitchen. Holding my arms down for so long, or holding something heavy—it’s too hard.
I wish everybody knew that if your body feels strange, seek help. You don’t know what it is—it could be anything. Especially if it’s something you haven’t experienced before. Don’t say, “Let me wait and see”—seek help immediately. That’s the key.
Next: How Heart Disease Affects Women Differently Than Men

For many, May marks the start of long-awaited warm weather, celebrating the first of many trips to the cottage, weekends spent in the garden or with friends at a park and, of course, time spent in the sun. There’s no denying a hit of vitamin D feels extra good after a dull few months, but when was the last time you thought about how those sunny days were affecting the health of your skin long-term?
Sun protection seems to be a low priority for many people above the equator. A survey* conducted in 2021 showed that 44 percent of North Americans experienced a sunburn that year. Yet, only 19 percent claimed they wore sunscreen daily, leaving those who didn’t at an increased risk of developing skin cancer—assuming they were applying and reapplying correctly.
To make sun safety a priority and remind people of its importance, Neutrogena®, a fan-fave brand in skincare, has partnered with Melanoma Canada to inform Canadians of good sun-protecting and skin cancer-detecting habits.
As we inch closer to summer, and with Melanoma and Skin Cancer Awareness Month arriving May 1, these partners are taking the opportunity to shed light on the seriousness of UV damage and melanoma, sharing every bit of information they can find under the sun (pun intended).

How the partners have—and will continue to—come together for Canadians
For years, people have relied on Neutrogena® for their tried-and-true personal care products that support overall well-being. From the brand’s SPF-packed skincare to their extensive line of broad-spectrum suncare products, they’ve established themselves as a trustworthy choice for keeping you and your skin safe.
The expert-led organization Melanoma Canada has also remained a reliable source for prioritizing the long-term health of Canadians. So it should come as no surprise that these partners have successfully launched many collaborative educational programs, community outreach initiatives, and social media campaigns.
Most recently, they hosted the 7 Summits Snowshoe Challenge for Skin Cancer in February and March 2023. This virtual and in-person event asked participants to snowshoe, bike, run, skate, or ski the distance equal to the seven tallest summits in the world, or as many as they could endure, all to encourage sun-safe activity during the winter. The challenge raised $185,193 for skin cancer awareness and reached the screens of over 26 million Canadians.
Beyond this event, the partners remain committed to promoting sun safety and skin cancer prevention year-round. After all, the sun doesn’t exclusively make an appearance during the summer (even if sometimes it may seem like it).
Neutrogena® provides continuous product and financial support for many of Melanoma Canada’s awareness events, including Strides for Melanoma—happening this year on May 28—while the organization helps promote the brand’s suncare and sun-safe initiatives to its community.

A quick refresher on what melanoma is, exactly
Melanoma is a cancer of the cells that produce melanin, the pigment responsible for giving skin its colour. When exposed to UV rays, the melanin naturally gets darker and causes the skin to tan or burn. The darker the skin cells, the greater their risk of forming abnormalities and spreading to other areas of the body.
Although melanoma is most common in people aged 15-49, it can affect any age and anyone regardless of sex or race. While it’s potentially deadly, it’s one of the most commonly diagnosed cancers as it’s often first visible on the skin. It’s also largely preventable with daily sun-safe practices and regular self-checks.
Your guide to the ABCDEs and 123s of melanoma
Doctors use the ‘ABCDE rule’ to identify abnormal characteristics on the skin. Doing this yourself at least once a month could increase your chance of catching something in the initial stages since melanoma has an 85 percent survival rate if detected early enough. Use this simple rule to keep a close eye on your skin and check for:
- Asymmetry in the shape of the spot
- Border irregularity that makes it look ragged, notched, uneven, or blurred
- Colour variety with shades of black, brown, tan, grey, pink, white, and sometimes blue
- A Diameter bigger than 6mm, which is the size of a pencil eraser
- Evolution in size, shape, or colour as a mole or lesion will change with time and may be itchy, scaly, or bleeding
Neutrogena® has also developed its comprehensive Skin Self-Exam Tool, which is easy to incorporate into your routine. The tool contains stats, tips, and other resources to help spot melanoma at home.
To ensure you’re covering your bases, Melanoma Canada created 3 Ways to Block the Rays, a campaign supported by Neutrogena®. The guide includes beneficial habits for keeping you protected. Even practicing just one of the three habits could go a long way.
- Apply sunscreen with at least 30 SPF every day, regardless of how much sun there is, as recommended by Health Canada.
- Wear UVA/UVB protective clothing.
- Seek shade during peak hours, typically between 11 a.m. and 3 p.m.

At the end of the day, your best offense is a good defense
Prevention is crucial in lowering your risk of skin cancer. With the leading cause being overexposure to UV rays, protecting your skin from potential damage is an absolute must. A single blistering sunburn before age 20 could increase your risk of developing melanoma later in life. So why not start taking care of your skin now?
When it comes to suncare, Neutrogena® has you covered—literally. Their best-selling Ultra Sheer Sunscreen line has non-greasy options for both your face and body. Not to mention that along with great coverage, they also boast a seamless, lightweight feel. But protection isn’t just about what you apply to your skin, it’s also about how you apply it and how much.
The experts at Neutrogena® say that to be properly protected you need to apply sunscreen 15 minutes before stepping into the sun for proper absorption and reapply it every two hours. They also say that the amount you should be applying is about the size of a golf ball for your entire body and the length of two fingers for your face.
Want more information on how to stay safe in the sun and decrease your risk of melanoma?
You can discover Neutrogena®’s range of sun-protective products and daily suncare habits at www.neutrogena.ca/sun and learn more about Melanoma Canada and their awareness initiatives at www.melanomacanada.ca.
*Data on File, Johnson & Johnson Consumer Inc

There are many ways to build a family, and it’s important to continue raising awareness to normalize that.
“Many Canadians are affected by fertility challenges,” says Carolynn Dubé, executive director of Fertility Matters Canada, “And these statistics don’t account for aspiring single or LGBTQ+ parents, all with the same goal of building a family.”

Fertility Matters Canada (FMC) is the leading national patient-focused organization providing free support, public education, and advocacy for equitable access to fertility care in Canada. Fertility Matters Canada supports those who are considering their future fertility, are currently on a fertility journey, are facing childlessness after infertility, have experienced a miscarriage or loss, or are seeking support or information.
There are many factors that can impact the journey to parenthood — and every journey is different, each with a unique set of challenges, an overwhelming amount of information, and difficult decisions to be made. It can lead to people going through this process feeling lonely along the way, not to mention emotionally and physically drained.
June is World Infertility Awareness Month, a globally celebrated moment that focuses on increasing awareness on numerous infertility issues faced by aspiring parents in Canada and across the globe. Organizations like Organon Canada, a leading women’s healthcare company, and Fertility Matters Canada are working to spotlight the stories of aspiring parents, sharing their fertility challenges and lessons learned. “We’re committed to turning the infertility narrative on its head and redefining (in)fertility to put a positive spin on an often-heavy conversation and to be more inclusive of all fertility stories and journeys,” says Dubé.
Anne-Marie Luca and Tayyaba Mohsin are two Canadian women working to break the stigma that prevents people and families from having open conversations about fertility and seeking the support they need.
Anne-Marie Luca
Anne-Marie is the founder of Info-Procreation, an organization that supports people experiencing infertility and members of the LGBTQ+ community on their fertility journey. Her personal fertility journey began when she was diagnosed with cervical cancer and needed a hysterectomy at age 35. After her procedure and cancer treatment, surrogacy was her only option to conceive a biological child. Surrogacy is anything but a straightforward process, and Anne-Marie was given only bits of information. So, she completed hundreds of hours of her own research to make her dream of having a family come true.

Tayyaba Mohsin
Tayyaba is a first-generation visible Muslim immigrant and an advocate for accessible fertility care and decreased stigma about infertility, especially for women of colour. She is also the founder of the OPS Fertility and Pregnancy Loss Group, an informal, employee-run group for all Ontario Public Service (OPS) workers who are seeking support for themselves or would like to join as allies. The group’s aim is to be a safe place for support, to consider potential improvements to OPS policies, and to promote understanding and provide education in the OPS. Tayyaba was diagnosed with Polycystic Ovarian Syndrome (PCOS) in her twenties, and experienced five years of infertility and pregnancy loss before undergoing IVF and an auto-immune treatment. She was able to conceive her daughter in January 2023.
Here, they open up about their journeys to parenthood.
What are some of the barriers people face in accessing fertility care?
Fertility clinics are busy—and waiting for an appointment can be stressful. Anne-Marie says her journey took almost two years, and even after getting into a clinic, she wasn’t given the attention she needed. “When my husband and I were in the middle of our treatments and had questions, it was tough to get a hold of the fertility team at the clinic because they were so busy,” says Anne-Marie. “That was a source of immense stress.”
Another major barrier to accessing fertility care? Expense. Tayyaba says when she and her husband first started trying to conceive, they were both in school, and the provincial plan didn’t cover fertility care for international students. “We struggled to find doctors and healthcare that were accessible and not an out-of-pocket expense to us,” she says. “Often there are surprise costs too like travel, missed work and unexpected treatment costs – they all add up and few are covered by the province.”
How can fertility care providers be more inclusive to all aspiring parents?
There needs to be greater awareness of how fertility affects different groups of people. “When we talk about fertility, we’re usually talking about reproductive fertility and missing a group of individuals in the LGBTQ+ community,” says Anne-Marie. Fertility care providers need to be more conscious of this and offer the resources necessary to assist with all types of fertility journeys.
As a member of the South Asian community, Tayyaba doesn’t feel represented by the fertility images and messaging typically seen in social media posts, brochures or posters on a clinic wall. “Fertility has a very white, straight face to it,” says Tayyaba. “It makes you feel like you’re facing this alone.” Tayyaba further notes that cultural and anti-racism competency and capacity training for all fertility care employees would go a long way in improving the fertility experience for people of colour, LGBTQ+ people and other underrepresented groups.
How can people trying to build their families find community?
Many people who have encountered challenges with starting a family are opening up about them via in-person and online communities. Anne-Marie started her fertility support group, Info-Procreation, after a psychologist at her fertility centre suggested she help other couples who are interested in having a baby via surrogacy. “Considering the lack of support groups, I wanted to provide guidance and support to individuals who struggle with infertility and those who identify as LGBTQ+.”
Tayyaba recommends reaching out to your fertility clinic, most of which have existing Facebook pages where people can find support and resources. Reaching out to your reporting manager, HR, or your union representative can be another important source of support. “You just can’t go through this experience without support from your workplace,” she shares. That’s why Tayyaba founded the OPS Fertility and Pregnancy Loss Group, a support group for Ontario Public Service employees.
What supports do you wish had been available when you began your journey?
Overall, people going through fertility challenges need more accessible information about their options and what they can expect—and they need healthcare providers to educate them on a range of fertility options. “Surrogacy is not very common or regulated, and there’s little reliable information available,” says Anne-Marie who had to do her own extensive research to get the information she was looking for.

Tayyaba wishes she had access to a fertility specialist earlier on in her journey. In addition to PCOS, Tayyaba also suffered from auto-immune related infertilty, which is experienced by only a small percentage of the fertility population. “I had to advocate for myself, consult with more than eight doctors, read numerous books and articles and speak to many fertility specialists to get answers,” she shares. It was a collaborative approach between her fertility doctors and reproductive immunologist that helped her to conceive her daughter.
There’s also a need for mental health support. “Providers need to prioritize the mental toll this journey can take on a person,” says Tayyaba. “It affects partner relationships, family relationships, and merges into all areas of life between work and home.”
Are there any moments of joy in your fertility journey you would like to highlight?
No matter what your journey looks like, there can be pleasant surprises along the way. Anne-Marie was amazed that despite having her son via surrogate, she was able to breastfeed.
“The amount of support I have received through friends found via support groups and at work is something I treasure the most,” says Tayyaba. “They celebrated my wins and supported me immensely when I was going through a hard time.”
For more information about Fertility Matters Canada and infertility support in Canada, visit Fertility Matters Canada at fertilitymatters.ca.

You deserve to feel amazing. And if you don’t—whether your digestion is out of whack or you’re fatigued most days of the week—there are steps you can take to feel better. First things first: Take a look at your diet and all the ways it can impact your well-being.
1. Prioritize gut health.
The microbiome of your gut is full of trillions of bacteria and an imbalance of microbes can cause a whole host of health issues like bowel problems and weight changes.

To keep your gut in check, you may also want to take a probiotic like Culturelle® Women’s Healthy Balance, which is specifically formulated by women for women. It helps to support digestive, immune and feminine health with a clinically proven blend of four lactobacilli found in a balanced female microbiome, plus Lactobacillus rhamnosus GG—the number one clinically studied probiotic strain in the world.† Take one capsule daily. (It’s 100% vegetarian, non-GMO and contains no synthetic preservatives, yeast, wheat, gluten or soy!)

2. Promote better energy.
Your to-do list is long and trying to get everything done while feeling sluggish will make each day feel like a chore. To improve overall energy levels, exercise and protect your sleep schedule, but also look to the foods on your plate. Insufficient iron and vitamin B12 can leave you feeling fatigued, so ensure you’re eating enough meat, fish, eggs, dark-green leafy vegetables, legumes, nuts and seeds. You may also want to take iron and/or vitamin-B-complex supplements to improve your levels.

3. Regulate hormones.
Puberty, pregnancy and perimenopause are all parts of life that can affect your hormones. (Of course, stress can do a number on your hormones, too!) Though you may not be able to control your life stage, you can monitor the foods you eat to get enough protein (for the amino acids), healthy fats (like omega-3s) and fibre, plus lower your sugar intake. Especially if you’re going through perimenopause, you may want to take fish oil supplements, which contain omega-3 fatty acids that benefit low mood and heart health.

4. Strengthen bones.
Osteoporosis is more common in women than men, but it’s possible to reduce your risk. Weight-bearing aerobic activity and resistance training can help to strengthen bones, as can eating foods rich in calcium (or taking a calcium supplement). Vitamin D is also essential for healthy bones and is made in the skin following sun exposure and is found in oily fish, red meat, egg yolks and vitamin-D-fortified foods.
For 25 years, Culturelle® Probiotics have helped individuals, children and families better support their digestive, immune, feminine and pediatric health. For more information about Culturelle®’s lineup of probiotics, visit culturelleprobiotic.ca.††
† Based on the number of Lactobacillus rhamnosus GG clinical studies, as of February 2023.
†† Culturelle® is a trademark of DSM.
Antidepressants are commonly prescribed to treat depression and anxiety—about 13 percent of Canadians take them, according to a small 2021 study. “They were designed to increase the release of specific neurotransmitters [like serotonin, norepinephrine and dopamine] in certain areas of the brain to help restore the imbalance and improve communication between neurons to treat symptoms of depression,” says Dr. Melanie McLeod, a board-certified psychiatric pharmacist. While physicians and researchers know this “correlates with improvement in depressive symptoms and brain functioning,” says McLeod, they still don’t fully understand how much of the improvements in mood are the result of the drugs, and why some patients respond preferentially to certain antidepressants versus others. These unknowns are one of several reasons why doctors need to recommend various antidepressants to patients to find the one that works with them.
(Sign up for our Must Reads newsletter for more feel-good tips, beauty product recommendations and delicious recipes!)
In other words, antidepressants are not a one-size-fits-all treatment. A doctor or healthcare professional should examine a patient’s symptoms and medical history and tailor the treatment options to suit their specific needs, says McLeod. There are also many factors to consider when prescribing antidepressants, including tolerability, side effects, the patient’s symptoms (for example, choosing a medication with a sleep-promoting agent for someone experiencing insomnia), safety considerations related to other medical conditions, risk of drug interactions, patient preference, cost, and safety for specific individuals, age groups or illnesses. She says that, for women, there are additional considerations related to menstruation, pregnancy and lactation.
What’s more, there are different classes of antidepressants to consider. Many inhibit reuptake, which is the process where neurotransmitters are naturally reabsorbed back into nerve cells in the brain. A reuptake inhibitor prevents this from happening to increase neurotransmitter activity. Selective serotonin reuptake inhibitors (SSRIs) increase levels of serotonin in the brain while serotonin and norepinephrine reuptake inhibitors (SNRIs) increase both serotonin and norepinephrine. Norepinephrine and dopamine reuptake inhibitors (NDRIs) increase norepinephrine and dopamine. Tricyclics also impact serotonin and norepinephrine, but are less selective than SSRIs. They act on receptors throughout the body.
Here’s a rundown of the pros, cons and common side effects of some often-prescribed antidepressants. They’re sold under multiple trade names, but all are available in generic format, which tends to cost less.
(Note that discontinuation symptoms—such as nausea and difficulty sleeping—may occur with any of these medications when stopped abruptly.)
Escitalopram (Lexapro)
Pros: An SSRI often prescribedl for anxiety and depressive symptoms. Along with other SSRIs, it’s considered a top choice by some for use during pregnancy and lactation.
Cons: Potential for sexual dysfunction and weight gain.
Possible side effects: nausea, headache, dry mouth, dizziness, weakness, excessive sweating
Sertraline (Zoloft)
Pros: An SSRI that is used to treat depressive symptoms and other mental health conditions like obsessive-compulsive disorder (OCD) and panic disorder. Generally considered safe for use in pregnancy and lactation. Less expensive than other medications.
Cons: Potential for sexual dysfunction.
Possible common side effects: Nausea, sleep issues, headache, diarrhea, loss of appetite, dry mouth
Duloxetine (Cymbalta)
Pros: An SNRI used for anxiety and depression. It can also be used to treat pain from medical conditions like fibromyalgia and diabetic neuropathy.
Cons: Potential for severe drug interactions.
Possible common side effects: sleepiness, headache, insomnia, dizziness, blurred vision, diarrhea, lack of energy, constipation
Venlafaxine (Effexor)
Pros: An SNRI prescribed for anxiety and depression, and generally well tolerated. May help reduce menopause-related hot flashes.
Cons: Safety concerns to consider with pregnancy.
Possible common side effects: nausea, sweating, headache, drowsiness, dry mouth, dizziness
Bupropion (Wellbutrin, Aplenzin, Zyban)
Pros: An NDRI used for depression, seasonal affective disorder and smoking cessation. It may help improve focus, concentration and motivation, and help with coping with fatigue.
Cons: May be too stimulating for some; may aggravate anxiety symptoms and insomnia. Not always suitable for those with an eating disorder or who are prone to seizures.
Possible common side effects: agitation, drowsiness, difficulty falling asleep or staying asleep, dry mouth, dizziness
Mirtazapine (Remeron)
Pros: A tetracyclic drug used to treat symptoms of depression and anxiety. Promotes sleep and improves insomnia with low reports of sexual dysfunction. It can also increase appetite, which is beneficial for individuals who are underweight.
Cons: Its strong sedation effect causes excessive tiredness. Some experience unwanted weight gain. Can, on rare occasions, cause changes in menstrual cycle, which is considered to be a severe side effect.
Possible common side effects: dry mouth, headache, sleepiness, nausea, vomiting, diarrhea, constipation
Vortioxetine (Trintellix)
Pros: An SSRI that also modulates serotonin receptors. It’s used to treat major depressive disorder and has been shown to be helpful with improving cognitive impairment associated with depression. Low reports of sexual dysfunction and weight gain.
Cons: It can be expensive compared to other antidepressants. Nausea is quite prevalent in the first two weeks of treatment.
Possible common side effects: nausea, constipation, vomiting, dizziness, dry mouth, diarrhea, headache
Next: Frustrated Your Antidepressants Aren’t Working? Here’s What You Need To Know
The #flawless nature of social-media filters has left many desiring a skin texture that’s completely smooth and pore free—impossible IRL. But Elizabeth Layton, regional education trainer at M.A.C Cosmetics, says that large pore size has actually long been a concern in the makeup chair. People commonly complain that they see their pores as large and have been unable to diminish their appearance with skin care and makeup, says Layton. “They often fixate on these perceived ‘flaws’ rather than celebrating their beautiful features.” She adds that all of this constant exposure—both to highly edited images and ads for products that falsely claim to completely erase pores—doesn’t help. The images set “an unrealistic expectation for the consumer who now expects near-instant results.”
(Related: How’s Your Skin Barrier Doing? (Here’s How to Know)
It’s important to remember that our pores do in fact serve a very important function. Dr. Geeta Yadav, board-certified dermatologist, and founder of FACET Dermatology in Toronto, explains that these tiny openings on the skin’s surface are connected to the sebaceous glands (the organ that secretes sebum) beneath, and function as release valves to allow sebum to flow to the skin’s surface, keeping it balanced and nourished. Unfortunately, pores can expand over time. “As skin becomes more lax with age, so do the pores on your skin,” Yadav says, adding that pores can also become larger when they are congested with sebum.
But, there are some strategies for maintaining or temporarily reducing pore size and a glut of new pore-minimizing products to choose from. “Skin-care formulas can reduce the appearance of pores, but not necessarily shrink them permanently once they have been dilated,” Yadav says. She recommends using products with salicylic acid, also known as beta-hydroxy acid, an oil-soluble ingredient that can go within the pore where it breaks down excess sebum that may be causing congestion. “By doing this, sebum can effectively and smoothly flow through the pore rather than worsen any blockages,” she says. Retinoids can also help, particularly when large pores are caused by weaker and oily skin. They regulate oil production while helping to strengthen the skin and promote collagen production, says Yadav.
At dermatologist offices, professional treatments like laser skin resurfacing and microneedling are the most popular in reducing pores. Yadav says they work by causing intentional, controlled damage to skin that stimulates collagen production. “When the laser damages the skin, your skin goes into overdrive with its natural healing response, generating new collagen which will help firm up the look of pores.”
Makeup can also diminish the look of pores through light-refracting and blurring effects. M.A.C’s Layton suggests following a hydrating skin-care routine, as makeup wears better on moisturized skin, and applying a primer before foundation. “When seeking a foundation to minimize texture, I suggest products that blur and trick the light—almost mimicking a filter,” she says. “Use it all over the face to even tone or spot-cover to address the areas where you want more blurring.”
One of Layton’s pro tips to soften the appearance of large pores is to apply powder, which she points out is also a great choice for those who don’t want to wear foundation. “The new generation of powders are refined, gentle and non-drying, leaving skin with a weightless blur,” she says. Her top pick? M.A.C’s new Studio Fix Pro Set + Blur Weightless Loose Powder, a light-reflecting setting powder with a matte finish. “It’s so soft, blurs and smooths the look of pores and creates a breathable veil,” Layton says. “It’s like your skin but better.”
Our top skin care and makeup picks for minimizing large pores:

Origins Clear Improvement Active Charcoal Mask to Clear Pores, $39.50, origins.ca

Dermalogica Porescreen SPF 40, $77, dermalogica.ca

Skinceuticals Silymarin CF Salicylic Acid Acne Treatment, $182, skinceuticals.com

M.A.C Studio Fix Pro Set + Blur Weightless Loose Powder, $44, maccosmetics.ca
Next: The Best Skin Care Routine for Your Age, According to Dermatologists
On a recent Wednesday night, feeling peckish and bored, I ordered a pizza and my situationship (a.k.a. the person I’m sort of dating) over to heat things up. We ate said pizza, drank some whiskey, and eventually slithered away to my bedroom.
It was my first time hooking up with this particular partner, and one of the few times I didn’t jump into bed on the first date. In other words, there was a fair bit of pent-up energy between us, which transpired into an evening of unexpected sexual acrobatics. It was a night that had it all: missionary, doggy, cowgirl, you name it. But none seemed to scratch my itch—until he rearranged my limbs, and entered me with that same satisfying feeling of sliding in a final puzzle piece. What was this position that felt just right? A buzzy move called “the pretzel dip,” which happened to be on my sex to-do list.
(Related: The Absolute Best Sex Position, According to Experts)
Here’s how the move went: I lay on my right side, and he kneeled down, straddling my right leg. I wrapped my left leg around his torso and thrusted and grinded, and we used our hands to please each other further. We kept eye contact the whole time, dirty talking while tangled up together. Orgasming was easy, and every part of my body felt pleasure.
According to Rashida Ahmed, a Toronto-based sex educator and intimacy coach, the pretzel dip promotes greater intimacy than most other positions because it allows for greater eye contact and hand play, since you don’t need to hold yourself up. “Plus, for those with vaginas, there are a lot more nerve endings near the opening of the vaginal canal, so a position like the pretzel dip can allow for more direct clitoral stimulation,” says Ahmed. It can also be a great position for a partner who isn’t well-endowed or is average-sized, as it allows for deep penetration.
The pretzel deep also allows you to get deep, emotionally. My partner and I talked through each move and ended up discovering what pleases each other most. Thanks to all the eye contact, all other noise in the room disappeared and we were fully focused on each other. Ahmed says the pretzel dip is a common tantric sex exercise that she recommends to her patients. The position (even for couples who are fully clothed) creates a closeness where they can feel literally intertwined, synchronize their breathing and thereby connect more deeply.
What’s more, the position is gentle enough for someone like me who has PCOS and can experience pain from sex. According to Ahmed that’s because it’s not high impact, and can therefore be an ideal move for a range of people, including those with mobility issues.
But the position might not be comfortable right from the start. If not, Ahmed suggests trying different angles, straightening the leg if need be, and also bringing in pillows underneath the hip (as I did). You may also want to change your location, such as opting for a couch or a flat surface like the floor for more support, as additional bounce might just be too painful for those with hip issues. I used an especially fluffy comforter to wrap around us so we were padded in every direction.
No matter how you slice twist it, the pretzel dip gets the job done—and quickly, effectively, and repeatedly. “You can really allow yourself to have multiple orgasms with it,” says Ahmed, because it stimulates a lot more of the vulva and penis than other positions.”
Next: 18 Goodies That’ll Help Turn Up the Heat in the Bedroom
Pad gaprao, sometimes written (incorrectly) as pad kra pao, is a true staple of the Thai diet. It’s sold by street vendors and at fancy restaurants, and made at home all over the country. I call this the “old school” version because it’s the old style that differs from the newer variants that are more popular today. It’s much simpler, seasoned with only fish sauce, and has no vegetables, so the flavor of the basil really shines. Modern variations include soy sauce, oyster sauce, and veggies like onions and long beans. There’s no wrong way to do it, and I want to share this piece of history before it disap- pears—and also because it’s much simpler to make than modern versions, but equally delicious!
Old-School Pad Gaprao
Pad Gaprao Moo Kai Dao | ผัดกะเพราหมูไข่ดาว
Serves 4
Cooking Time: 10 minutes, plus 5 to 10 minutes if frying eggs
Ingredients
- 2 to 3 Thai chilies, or as many as you can handle
- 1/3 cup (40 g) chopped mild red peppers
- 7 cloves (35 g) garlic
- Oil for frying eggs (optional)
- 4 eggs (optional, see note)
- 2 to 3 tablespoons (30 to 45 ml) neutral oil
- 1 pound (450 g) lean ground pork
- 2 tablespoons (30 ml) fish sauce
- 2 teaspoons (10 ml) granulated sugar
- 1½ cups (22 g) holy basil or Italian basil leaves (see note)
- Jasmine rice, for serving
Notes: Pad gaprao is typically paired with a fried egg when served as a one-dish meal. If serving as part of a multi-dish Thai meal, you can omit the egg.
You might be tempted to use Thai basil instead, but Italian basil is actually the better substitute.
Directions
Using a mortar and pestle, pound the Thai chilies until fine, then add the mild red peppers and garlic and pound into a rough paste.
If you’re making fried eggs, make them now. In a small nonstick frying pan, heat about 1/3 inch (8 mm) of oil over medium-high heat. Test the temperature of the oil by adding a little piece of vegetable scrap, like the garlic or pepper, and it should bubble excitedly right away. Once the oil is hot, add 1 egg. The white should bubble up right away. Using a spoon to occasionally baste the top of the egg with oil to help it cook faster, cook for about 1 minute for a runny yolk, or 2 minutes for a set yolk. You want the white crispy and browned, so if it’s not browning, turn up the heat. Remove the egg from the pan and drain on paper towel; repeat with the remaining eggs.
Place a wok on medium heat, then add the oil and garlic-chili paste. Stir for about 2 minutes, until the smallest bits of garlic start to turn golden.
Turn the heat up to high, add the ground pork, then quickly toss to mix with the garlic-chili paste. Add the fish sauce and sugar, and keep tossing and breaking up the pork until it is fully cooked.
Turn off the heat, then add the holy basil and cook just until wilted. Taste and adjust the seasoning with fish sauce and sugar as needed.
Plate and serve with jasmine rice. If serving as a one-dish meal, place the rice on a plate, spoon the pork over it, and top everything with the fried egg.
Tip: I usually say you can make things as spicy as you want, but for the real pad gaprao experience, you should make it as spicy as you can handle! But it’s not just about the heat, as chilies also provide flavor that’s important to this dish. This is why we use mild and hot chilies; the mild ones add the needed chili flavor without making the dish too spicy. Red bell pepper will work, but preferably something smaller and less watery. The seeds and pith can be removed to reduce heat.
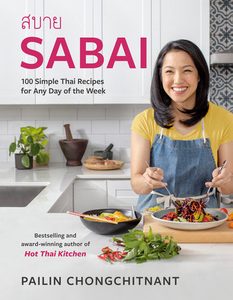
Excerpted from Sabai by Pailin Chongchitnant. Copyright © 2023 Pailin Chongchitnant. Photographs by Janis Nicolay. Published by Appetite by Random House®, a division of Penguin Random House Canada Limited. Reproduced by arrangement with the Publisher. All rights reserved.
Next: How to Make Egg Fried Rice (And Use Up Fridge Leftovers)
As more and more people have learned about the benefits of nasal breathing, the trend of mouth taping has taken off, and it’s not just for bio-hackers and those susceptible to wellness fads. Driven by social media, this health trend has resulted in many people—mainly TikTok users—taping their mouths shut at night (yes, really) to stop them from breathing through their mouths.
While many online health hacks are baseless, this one isn’t quite as bizarre, dangerous or ill-advised as it may sound. The importance of breathing through your nose at night shouldn’t be discounted, as anyone with sleep apnea or a snoring issue (or who shares a bed with someone who struggles with these issues!) might already know. That’s because nasal breathing provides a number of health benefits, while mouth breathing is associated with a list of potential problems.
Why breathing out of your nose is better than mouth-breathing
Nasal breathing allows an individual to breathe more slowly and effectively. The nose is designed to filter viruses, bacteria, debris and allergens, says Sabrina Magid-Katz, a New York-based dentist who specializes in sleep dentistry and related sleep disorders. “People are finally starting to think about what some ancient cultures have always known—that breathing in and out through the nose is healthier,” says Magid-Katz, referencing the nasal breathing exercises taught in yoga and Tai Chi classes.
The nose humidifies the air we breathe, and also increases oxygen to the bloodstream, improves lung function, and decreases stress on the body. The body’s cells are able to get the oxygen they need more efficiently from the bloodstream, allowing the body to function optimally, the muscles to recover faster and the heart to work less hard. “Who wouldn’t want less stress and inflammation, and more stamina, energy and mental function?” she says.
On the other hand, mouth breathing causes dry mouth, according to Brian Rotenberg, a head and neck surgeon and a professor of Otolaryngology at Western University in London, Ont. This is because the mouth isn’t capable of humidifying air in the same way as the nose. Saliva typically washes bacteria from the mouth when it’s closed, but it can more easily survive and cause issues when the mouth is open and dry—potentially leading to bad breath, gum disease and cavities, he says.
Breathing dry air through the mouth can also cause inflammation of the airway and further block it, says Magid-Katz. This creates an airway that is more collapsible, which can lead to Obstructive Sleep Apnea (OSA) — a medical condition in which someone stops breathing while they’re sleeping, interrupting their sleep cycle and often decreasing the oxygen in their blood. This condition is associated with other medical conditions including high blood pressure, stroke and diabetes, she says, as well as chronic sleep deprivation or a sense of never feeling truly rested.
What causes mouth breathing?
There are a few different reasons why an individual might be a mouth breather, Magid-Katz says. Some people breathe through their mouth because their nasal passage is blocked as a result of allergies, and others do so due to a structural problem, such as a deviated septum. Mouth breathing often starts when we’re kids, she says, preventing muscular habits and dental arches from growing to properly support the nasal passage.
Enlarged tonsils and adenoids—as well as what’s called “soft tissue trauma,” often caused by snoring— can also block the airway, which only further encourages mouth breathing and, in turn, creates a vicious cycle of more trauma and enlargement. “Other people breathe through their mouth out of habit,” she says. “Interestingly, the less they breathe through their nose, the harder it may become.”
Signs you might be a mouth breather
If you constantly wake up with an exceptionally dry mouth or lips, or even a sore throat, Rotenberg says there’s a good chance you’re breathing through your mouth at night. Since some nighttime mouth breathers also breathe through their mouths during the day, you can try looking at photos or observing yourself in the mirror. “If your lips are parted or your mouth is hanging open, chances are you’re breathing through it,” says Magid-Katz. You can also self-assess your smile, as an extra gummy smile might mean you’ve been mouth breathing since childhood. Or, look at your posture from a side angle, or get someone to take a picture of you. Those with blocked airways, including mouth breathers, tend to have heads that reach forward because they’re trying to get more air. (Since most mouth breathing starts in childhood, our posture can naturally develop this way to accommodate the habit.)
How does mouth taping work?
The practice consists of using some kind of porous tape—not duct tape or masking tape—to keep the lips shut at night in order to encourage nasal breathing. Its appearance differs based on the brand, but mouth tape is often thin, transparent and can be applied horizontally, vertically or in a criss-cross shape across the lips. If you’re picturing looking like a hostage with tape across your mouth, you can take comfort in knowing the tape made specifically for this purpose doesn’t look quite as alarming as duct tape would – although it’s still slightly creepy and strange-looking. And while it will be more challenging to talk to your partner or take a sip of water in the night, mouth taping fans say the benefits can outweigh these minor inconveniences.
“If you are going to try tape, use one that is porous and is not too adhesive so that you can still open your mouth if need be,” Magid-Katz suggests. This way, she says, the tape is more of a reminder and less restrictive. Some users try basic surgical tape from the pharmacy. She recommends doing an initial trial run for a short period of time during the day or early evening, when you are awake and calm.
Once you apply the tape, put your tongue to the roof of your mouth and breathe through your nose slowly. You can even do this with the help of a meditative breathing app.
“If it does not feel right for you, don’t do it,” she says. “Most importantly, always make sure you are able to breathe through your nose safely.”
According to Magid-Katz, some people do find mouth taping combined with over-the-counter nose strips (which are worn outside the nose and help open the sinus passages) to be effective. (You can also use nasal dilators, which go inside the nostrils.)
And while Magid-Katz says mouth taping could work for some, Rotenberg says he’s “firmly against mouth taping.” That’s because mouth breathing is usually caused by some kind of obstruction, so taping the mouth shut without an understanding of what the source of obstruction is in the first place doesn’t really make sense. “It’s not as if you can psychologically trick yourself to overcome nasal allergies or a deviated septum,” he says.
What to do if you’re a mouth breather
Instead of mouth taping, Rotenberg says it’s a better idea to go see your healthcare provider to figure out what the actual source of the obstruction is and treat that instead. “There are lots of safe and proven solutions, you just need to have the correct diagnosis first,” he says. Allergies, for example, can be treated with nasal steroid sprays, while surgery is an option for polyps or a deviated septum.
Magid-Katz also recommends speaking to a physician or dentist who is knowledgeable when it comes to the airway. It’s important to make sure the nasal passage is clear and the dental arches allow for proper nasal breathing, she says, and you can also talk to a myofunctional therapist who can help strengthen and retrain the muscles. Some dental appliances are designed to help children and adults correct the habit as well. “For some people, the more they breathe through their nose the clearer and easier it gets, so the first thing to do is become more conscious of it,” she says. “Try setting your phone alarm periodically throughout the day as a reminder to think about whether your mouth is open and how you’re breathing, or have a friend or loved one look at you periodically and note if your mouth is open. Set aside time each morning and night to practice proper breathing techniques.”
Next: Can a Weighted Blanket with Cooling Tech Help Me Sleep (and Not Over-Heat)?