Beans are a staple in most cuisines around the world, and for good reason. They’re nutritious, affordable, convenient to make and comforting. Both canned and dried beans are a good source of plant-based protein, fibre and iron to keep you feeling energized and full over longer periods of time. Most beans are also an excellent source of potassium, which helps to keep blood pressure levels in check. Perhaps the best part about beans, though, is how easily they can transform from a plain pantry staple to a truly wonderful and satisfying meal.
The benefits of cooking with dried beans
It’s true that cooking dried beans may not sound that appealing—they can’t compete with canned when it comes to convenience. But for recipes where beans take centre stage, dried are well worth the extra time and effort. By adding your own seasonings from the start, you can impart big flavour and control the salt levels. (Canned beans contain added salt, which you can partially remove by draining and rinsing them, but it’s worth keeping in mind if you are looking to reduce your sodium intake.)
Dried beans lend themselves well to batch cooking, since it’s easy to cook up a large quantity at once, and you can freeze them after cooking to add to future meals. They also yield a cheaper cost per serving than canned. Another benefit to dried is texture: Dried beans maintain their shape better during cooking, while remaining soft and creamy on the inside, whereas canned beans tend to turn mushy and break down.
Choose your bean adventure
The same cooking method can be used for almost all dried beans, which can then be eaten as is, or added to soups and salads or blended into dips and purees. For saucy dishes where beans are the main attraction, I love a creamy, starchy white bean such as a cannellini, great northern or gigantes. For chilis, I’m partial to smaller and sturdier black beans, and my go-to for a low-effort curry is always quick-cooking, nutritionally dense red lentils.
(Related: How to Incorporate More Beans and Plant-Based Proteins into Your Diet )
Don’t forget to prep
Most dried beans benefit from a pre-cooking soak for a few reasons. Soaking the beans in water plumps them up, helps them soften and leads to a shorter cook time. Soaking also helps to wash away some of the compounds in beans called lectins that can create uncomfortable gastrointestinal effects like gas and bloating. For smaller, thin-skinned varieties like lentils, black eyed peas and split mung beans, you can skip the soak and opt for a rinse instead—it will still help reduce the lectins.
How to make brothy beans
At the minimum, you’ll want to add salt to season the beans from the inside out as they cook (ballpark about 1 tablespoon per pound of beans used). Salt also helps beans retain their shape during cooking, for a tender interior with a bit of resistance when you bite into it. You can throw in woody herbs like rosemary, thyme, bay leaf and oregano; leafy herbs like parsley, cilantro and dill; a halved lemon (try searing it cut-side down in a hot pan before adding it to the pot for extra flavour); onions or shallots; fresh or dried chilies; and even a hunk of smoked bacon or ham hock.
Once you’ve selected your cast of flavours, bring the pot of beans to a simmer, and cook over low heat until they’re cooked through and tender. Don’t rush this process: Amping up to a boil will make the beans tough and cause their skins to split. Once cooking is complete, you can add in acidic elements like a splash of vinegar or lemon juice to brighten things up (adding them too early in the cooking process can prevent beans from softening). To make your broth extra creamy, stir a spoonful of aioli or an egg yolk into the hot liquid right after plating into bowls.
Once cooked, store beans in their cooking liquid in the refrigerator to prevent them from shriveling, or freeze them for meals down the line. That cooking liquid is a highly flavourful, aromatic broth, so save it to use as the base of soups, in braises or as a replacement for pasta water to thicken pasta sauces.
After my first bowl of creamy, brothy beans, I was hooked. The perfectly seasoned leftovers in the freezer I used for minestrone the following week clinched it: Consider me a dried-bean convert.
Next: How to Make Pizza Beans, an Easy Protein-Packed Side Dish
You might have noticed a new fitness trend popping up on your social media feed—wall Pilates. While celebrities and influencers have long credited standard Pilates workouts for their sculpted bodies (hello, Kate Hudson and Jennifer Aniston), the latest viral TikTok trend is a new variation on this classic workout.
To get the scoop on what wall Pilates is all about, we talked to certified Pilates instructor Sarah Micak, who works at Body Harmonics, a movement studio in Toronto.
(Related: What Trainers Want You to Know Before You Take a Class)
What is wall Pilates?
“Wall Pilates is really just using the wall as a prop, which is something Pilates instructors do all the time,” says Micak. “We use the wall for feedback because it helps you figure out where your body is in space, it can activate deep core muscles that support the spine and because it provides resistance,” she explains.
Wall Pilates looks a lot like classic Pilates, a workout popularized in the 1920s by Joseph Pilates. It involves standard moves like glute bridges, leg lifts, planks, push-ups and ab-strengthening “hundreds,” where exercisers use breathwork to focus on their core while pumping their arms up and down. All of these moves are, you guessed it, performed against a wall.
For example, instead of doing a bridge with your feet on the floor, you would brace your feet against the wall to target your core and back in a different way. (If you’ve seen how-to videos on social media, there’s a lot of hip thrusting involved.)
Why is the Pilates wall workout so popular right now?
“Pilates is low-cost and easy to do at home, so using the wall is one way to keep things fresh and new,” says Micak. “Pilates and at-home props really exploded over the course of the pandemic because people needed to get creative. Instructors used dining chairs, walls, or even cans of food in their workouts and that creativity has continued,” says Micak.
With the popularity of FitTok, YouTube and Instagram workouts, everyone has access to multiple fitness options, so people are looking for more variety in their workouts. The workouts are often quick, too, clocking in at less than 20 minutes. It’s also low-impact, which means it’s fairly easy on your joints. And because it’s not as sweaty as, say, going for a run, it’s more manageable to sneak in a wall workout before heading to the office or during a WFH lunch break. Plus, if you can suss out the best virtual workouts, wall Pilates costs next to nothing.
Do you need any equipment?
Pilates in general requires little to no equipment to get started. Ideally, you’d have a yoga mat and enough space so there are no obstacles on the wall and its surrounding area. One of the things you’ll immediately notice is that it takes some practice and adjusting to master the moves, which may require more space than you think. For example, during a glute bridge with your legs on the wall, you may be constantly scooting your butt closer to the wall to get your legs into the right position.
Is wall Pilates good for you?
Pilates in general has a lot of benefits because it focuses on those deep core muscles that you use to support your body every day, says Micak. Whether that’s carrying your kids or picking up groceries, you need a strong core to get through daily life without injury. “One of the great things about using a wall is that it provides resistance, a little like the Reformer [a Pilates machine], to make your exercises more challenging but more supported, so you can work the body in a new way and really tailor your workout,” she explains. But just because some of the moves might look simple, that doesn’t mean they are. (Don’t be discouraged if you can’t do a plank with your feet on the wall on the first try—or ever!)
What should you look for in a wall Pilates workout?
When you’re looking for a wall Pilates video to try, do some basic research first. “Be smart about who you’re taking instruction from,” recommends Micak. “Is it someone who is certified in Pilates? The more training the person has, the safer the movements will be in general.” Look for certifications, read the user comments, and even watch the full video in advance of trying it if you have time.
Will it help with weight loss?
Be warned: When you search wall Pilates, you’ll be bombarded with toned abs, round butts and a lot of talk about torching calories. While sticking with any exercise program could help you see these kinds of results, weight loss isn’t—and probably shouldn’t be—the focus of Pilates, says Micak. The standard benefits of Pilates are strengthening your core and muscles overall, and creating alignment in your body.
And what about the popular 28-Day Wall Pilates challenge that’s all over your social channels? “In theory, you could do Pilates every day,” says Micak, “but realistically, doing it three times a week is probably a really great goal.”
Where can I find the best free wall Pilates workouts?
There are a few popular subscription wall Pilates programs and paid apps, or you can watch reels on Instagram and TikTok to cobble together a workout. But we did our research and found some great free full-length videos on YouTube created by certified Pilates instructors.
We recommend trying Callie Jardine’s 10 Minute Full Body Wall Pilates for Beginners for an accessible, short workout or Rachel’s Fit Pilates Wall Pilates Beginner Workout. Both of these videos have over 1 million views and the instructors provide detailed instruction. In addition, they provide free programs to follow on their YouTube channels.
Other great (and free!) options to try include LivAligned Pilates, Wall Pilates Workout 20 Min Full Body, Jessica Valant Pilates 15-Min Wall Workout for Beginners or Trifecta Pilates Beginner Wall Pilates 20 min at-home Workout.
Next: Pilates Isn’t Only Good for Your Physical Health—But Your Cognitive Health, Too
Recent research highlights that the timing of our meals, particularly the last one of the day, can significantly affect our health. The story is not merely about what we consume, but also about when we do so. The debate about dinner timing finds substantial scientific backing with a Brigham and Women’s Hospital (BWH) study published in Cell Metabolism in October 2022, suggesting that early dinners could have more health benefits than previously believed.
The science of early dinners
Senior author of the study, Frank A. J. L. Scheer, director of the Medical Chronobiology Program in BWH’s Division of Sleep and Circadian Disorders, explained the study’s objective in a press release: “We wanted to test the mechanisms that may explain why late eating increases obesity risk.”
The study defined an early dinner as a meal consumed three to four hours before bedtime, aligning with our body’s circadian rhythm. This time management allows the body to efficiently digest food, process nutrients, and smoothly transition into a fasting mode during sleep, facilitating essential restorative processes (and arguably better sleep, according to some experts).
The benefits of an early-bird dinner
The BWH study discovered stark differences in metabolic profiles of early and late diners. Early diners demonstrated lower blood glucose levels, improved fat-burning capacity, better sleep quality, and higher energy levels. Meanwhile, late dinners led to increased hunger, slower calorie burning, and elevated fat storage, posing risks for conditions like diabetes and cardiovascular disease.
Further reinforcing these findings, a study published in Obesity Reviews examined the effects of energy intake distribution on weight loss. This systematic review evaluated nine randomized controlled trials and concluded that focusing on earlier energy intake resulted in significantly greater short-term weight loss. Alongside weight loss, improvements were observed in insulin resistance, fasting glucose and LDL cholesterol levels.
Implications and recommendations
These findings hold considerable implications for those dealing with health conditions like diabetes, thyroid issues, polycystic ovarian disease, and cardiovascular disorders. The studies spotlight the importance of early and light dinners, thus prompting a reevaluation of our dinner schedules and meal planning. As first author Nina Vujovic, put it: “Does the time that we eat matter when everything else is kept consistent? And we found that eating four hours later makes a significant difference for our hunger levels, the way we burn calories after we eat, and the way we store fat.”
Tailoring dinner time to fit your schedule
The exact timing of dinner isn’t a one-size-fits-all scenario, as people’s routines vary widely. Maya Feller, a nutritionist based in Brooklyn, NY, emphasizes that our schedules—ranging from traditional nine-to-five to round-the-clock—are pivotal when considering “ideal” meal times. Therefore, finding a dinner time that seamlessly fits into your schedule is essential, rather than adhering to a strict, potentially unfeasible timetable.
Registered dietitian Wendy Bazilian offers insightful tips for those whose routines may not accommodate an early dinner. She recommends consuming meals or snacks every three to five hours. This regular eating pattern can help stabilize blood sugar levels, preventing the onset of hunger pangs and energy lulls.
Furthermore, it’s advantageous to leave a gap of two to three hours between your last meal and bedtime. This gap ensures your body has sufficient time for most of the digestion process—letting you get adequate rest and repair during sleep.
The takeaway from these studies is clear: An earlier dinnertime might confer multiple health benefits, from metabolic health enhancement to improved sleep quality. It’s time to reconsider not just the contents of your plate, but also the clock. As research grows, it’s becoming apparent that understanding the interplay between our eating habits, their timing, and the body’s internal clock should be an integral part of our health strategies. After all, leading a healthy lifestyle isn’t solely about counting calories but also understanding when and how to fuel our bodies.
Next: It Might Be Time to Stop Worrying About Your Protein Intake
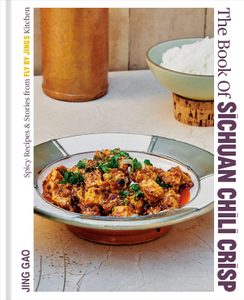
Happiness for me is slurping a deep bowl of these classic noodles—they’re an iconic Sichuan street food dish for a reason! They rose to fame in Chengdu, where they were sold by street hawkers, who carried their wares in baskets tied to bamboo poles (called dan in Chinese); hence, their namesake. Because they’re so famous, there are countless variations that have evolved from the original, from Taiwanese to Japanese versions. The beauty of these noodles is that they’re delicious no matter what, but these are the dan dan noodles I know.
An essential ingredient in dan dan noodles is yacai, preserved mustard greens. They add the necessary deep umami funk and crunch that make dan dan noodles so addictive. Yibin suimi yacai is the brand to get, but it can be hard to find. Try your local Chinese grocery store or search online. If you absolutely cannot find it, you can do without it.
Dan Dan Noodles
Serves 4
Ingredients
Meat Topping
- Neutral oil for frying
- 2 tbsp Yibin suimi yacai
- 115g ground beef or pork
- 1 tsp light soy sauce
- 1 tsp dark soy sauce
Sauce
- 4 tbsp Sichuan Chili Crisp
- 2 tbsp light soy sauce
- 2 tbsp dark soy sauce
- 1 tsp ground roasted sichuan pepper, plus more for garnish
- 4 tbsp thinly sliced scallions, green parts only, plus more for garnish
- 450g dried thin Chinese wheat noodles or noodles of your choice
Directions
1. To make the topping: In a wok over high heat, warm the oil until very hot. Add the suimi yacai and stir-fry for 1 minute, until fragrant. Add the ground meat and both soy sauces and cook for 5 to 6 minutes, until the meat is brown but not dry.
2. To make the sauce: In a small bowl, combine the chili crisp, both soy sauces, roasted Sichuan pepper and scallions. Divide the sauce evenly into four small bowls.
3. To cook the noodles: In a medium pot over high heat, bring water to a boil and cook the noodles according to the package instructions. Drain the noodles in a colander and rinse under cold water to stop them from cooking further.
4. When ready to serve, divide the noodles among the four bowls with the sauce and top with the ground meat. Garnish with the scallions and a dash of roasted Sichuan pepper.
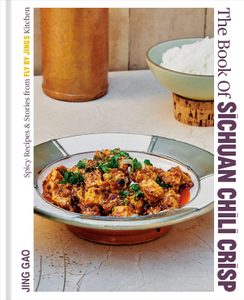
Excerpted from The Book of Sichuan Chili Crisp by Jing Gao. Copyright © 2023 Jing Gao. Photography by Yudi Ela Echevarria and Robert Nilsson. Published by Penguin, an imprint of Penguin Canada, a division of Penguin Random House Canada Limited. Reproduced by arrangement with the Publisher. All rights reserved.
Next: This Easy Brown Sugar Mochi Recipe Calls for Just 5 Ingredients
![Aveeno[58][90]](https://www.besthealthmag.ca/wp-content/uploads/1990/12/aveeno5890.png?fit=700%2C525)
Around a quarter of Canadian sensitive skin suffers have experienced eczema, with more than 85 percent dealing with burdensome symptoms, like itching and redness, every day. Of this group, 21 percent were those with darker skin tones.*
Yet, while most of the assessment and treatment protocols for eczema work well for light skin tones, they fall short for skin of colour.
To better understand this reality, Canadian skincare leader, the makers of AVEENO®, along with board-certified dermatologists, continue to build awareness around how eczema presents on different skin tones to close this educational gap in skin health.
Everything you need, all in one place
The AVEENO® Canada Skin of Colour Hub was created as a “one-stop shop”, sharing photos and symptoms of eczema, management options and more to support Canadians with skin of colour on their eczema journey.
Early this year, AVEENO® Canada released their #SkinVisibility table book, which documents lived experiences from patients, insight from experts, a portfolio of reference images and specialized care tips – all available on the AVEENO® Skin of Colour Hub. Beyond the tablebook, the hub is intended to be a resource for those on the onset of their eczema journey. It shares tools that allow everyone, regardless of colour, to identify symptoms, develop a management plan and find solace in their own skin.
![Aveeno Img2 1000x750[30]](https://www.besthealthmag.ca/wp-content/uploads/2023/12/Aveeno-IMG2-1000x75030-1.jpg?fit=700%2C525)
Let’s go back to the basics—what is eczema?
Dr. Sonya Abdulla, a double board-certified dermatologist in Canada and the US, describes eczema as a “chronic inflammatory condition characterized by inflamed, itchy patches on areas of the skin like the face and folds”. In light skin, she notes, the troubled areas typically appear red and scaly, while on darker skin tones, they appear with a purple to grey, or ashy hue.
Eczema is a result of a disruption to the skin barrier (the outer layer that retains moisture and protects us from irritants) and while the cause of eczema is mostly unclear, there are common triggers that people of all skin tones can pay attention to.
Things like extreme weather exposures—both hot and cold—fragrances, environmental allergens and pollutants, food sensitivities, friction and rubbing, even stress, can all contribute to the worsening of symptoms.
Some key markers for identifying eczema are extreme itching, thickened skin, darkness around the eyes, small bumps on the abdomen, arms, and legs as well as raised areas that develop around hair follicles, resembling goosebumps.
For skin of colour, though, there are other specific markers that aren’t well-identified or broadly discussed.
The diagnosis problem of eczema in darker skin
Dr. Geeta Yadav, a board-certified dermatologist and founder of FACET Dermatology, says a major concern for people of colour is the discolouration that occurs in the aftermath of an eczema flare-up, as a result of the inflammation.
With irritation-induced scratching, the affected area and surrounding skin develops hyperpigmentation that can last for months—even if the eczema has been treated. Since these pigmentary changes are so long-lasting, Dr. Yadav stresses the importance in diagnosing and treating eczema as early and aggressively as possible.
The problem is misdiagnosis, underdiagnosis or even no diagnosis have long been a barrier for treating eczema in skin of colour.
A key reason for this, according to the CDA, is physicians have historically been trained to diagnose eczema on white skin because that’s what they’ve studied in medical school textbooks. In fact, less than five percent of imagery found in these texts show conditions on non-white skin tones.*
This lack of inclusivity in educational resources is foundational for why skin of colour is not diagnosed or treated properly—leading to the resurfacing of the problems highlighted by Dr. Yadav. Without proper knowledge, doctors are less likely to diagnose the condition properly and those affected end up suffering longer-term.
Not only is “early intervention key to address symptoms and prevent long-term consequences [like discolouration], but also improve that person’s quality of life”, states Dr. Yadav.
Dr. Abdulla agrees and says that communicating your symptoms to your healthcare provider and the impact they have on your quality of life can go a long way in treating your eczema.
“Keep in mind, treatment success means improvement or resolution of the signs and symptoms”, says Dr. Abdulla. Since “itch is the predominant symptom seen with eczema, [and] much of the inflammation may be difficult to appreciate in darker skin tones, the degree of itch can help highlight the severity.”
Living with it—from a patient’s POV
Dermatologists insist that the difficulty in diagnosing eczema in skin of colour is common and that no one should feel they have to face it alone.
In fact, to underscore this, the AVEENO® #SkinVisibility tablebook shares stories of people in the community with advice for identifying and managing this skin condition.
Ruchika Karnani’s eczema was reported as almost exclusively stress-induced, with flare-ups worsening with changes to diet, environment, climate and ingredients. She shares that with her eczema presenting in unusual ways, she had to go through a lot of trial and error. While she waited for a diagnosis, she began to make small changes herself—reworking her diet and incorporating mindfulness practices in her daily routine.
“I [aimed] to keep my stress as controlled as possible while also living a generally healthy lifestyle to further reduce the risk of an outbreak”, says the woman. After four months of doctor’s office visits, prescription trials and holistic treatments, she finally received a diagnosis.
What she learned from this experience: “Expert opinions are crucial but often take time to get…so catering your daily routine to be in favour of healing in the interim, even in the smallest ways, can help mitigate factors that complicate the diagnosis process.”
For another patient, Natasha Kaycee, eczema was more than just a skin menace, it was a blow to her confidence. With random flare-ups that would disappear after weeks, her hard-to-diagnose condition was often conflated to dry skin in need of serious moisture.
She recalls the doctor viewing her eczema as ‘not a big deal’: “It took over two years to get diagnosed…when one doctor took my concerns seriously and evaluated me, [helping] me manage the flare-ups and avoid them as much as I can.”
Dr. Geeta Yadav also encourages seeking a second opinion. “Though it can feel intimidating to contradict a medical professional, it’s critical to advocate for yourself if you think something isn’t right with your treatment or care.”
You can read about more patient experiences in the AVEENO® #SkinVisibility tablebook, available for download in the hub.
So, where to go from here
While there is no single solution for dealing with eczema, there are a lot of coping strategies—whether it be limiting exposure to personal irritants, sticking to a skincare routine or practicing self-care. What’s important is finding what works for you.
The makers of AVEENO® have curated eczema identification and management tips for skin of colour that are easy to follow and implement. Not to mention, their Eczema Care line is well-known (and loved) by those dealing with this condition, thanks to the nourishing ingredients, like colloidal oatmeal and vitamins B and E, found in the formulas. However, you should consult with a healthcare professional for an official eczema diagnosis.
The makers of AVEENO® have shared some helpful tips for where to start:
- Simplify your skincare routine with barrier-targeted ingredients. Think: simple cleanser, followed by a moisturizer that will help restore hydration and rebuild resilience. A medicated moisturizer is considered first-line therapy for treating eczema.

Our Pick: Eczema Care Daily Moisturizing Cream
- Identify potential triggers and do your best to limit your exposure to them
- Shower in lukewarm, not hot, water
- Incorporate clinically-supported colloidal oatmeal to help strengthen the skin’s moisture barrier, soothe dryness, support the skin’s microbiome and provide temporary relief of symptoms

Our Pick: Aveeno®’s Eczema Care Itch Relief Balm
- Protect your skin from both hot and cold weather with the use of SPF in the heat, and outerwear accessories in the cold
Following these tips can not only improve your eczema but can also improve how much it interrupts your life. The greater awareness around diagnosing skin of colour with eczema and the community-powered confidence necessary to find peace with this skin condition, is exactly why the makers of AVEENO® developed the Skin of Colour Hub.
Find out more about this initiative at: aveeno.ca/skin-hair-solutions/eczema and aveeno.ca/skin-hair-solutions/eczema/skin-of-colour.
*In partnership with AVEENO® Canada, Leger conducted an online survey among a representative sample of 1,501 Canadians, 18+, who experience skin sensitivity in the summer and/or winter months. Respondents are members of Leger’s online panel. The survey was conducted in English. For comparative purposes, though, a probability sample of 1,501 respondents would have a margin of error of ±2.5 per cent, 19 times out of 20.
The autumn harvest is a bountiful time on the farm for Judy Ning and her husband, Hans. It’s their third fall season since they purchased a fixer-upper house on two acres of land outside Picton, Ont. and relocated their two kids.
They had endured the first pandemic lockdowns in Montreal, where they helped run a family-owned hotel. But Hans had always dreamed of living off the land and off the grid, and Judy wanted to reconnect with her heritage by cultivating Asian varietals descended from precious seeds her mother had brought from Thailand as a Hmong refugee decades ago.
Because the Nings had been camping at nearby Sandbanks Provincial Park for years, they were especially familiar with that part of Ontario, and started Paper Kite Farm in 2021. (The name is a nod to Hans’s family roots in China—because both paper and kites come from China, Judy explains.)
The seeds they use are hard to find in Prince Edward County, and they have quite the backstory. In 1986, as Judy’s mother travelled from Laos to Thailand to the U.S., she smuggled the original batch of seeds by sewing them inside the embroidery of her skirts. She then planted them in pots and pails and patches of grass between the pavement outside the public housing units in California where they were living as part of a refugee resettlement program. “Anywhere she could find a little bit of green,” says Judy. “And they’ve always been with me—everywhere we moved.”
While there are plenty of farms in Prince Edward County, the crops are fairly homogenous, says Judy. “Everyone’s growing the same things.” The Nings bring something different to the market, and it’s personal.

“When I came to Canada, I was the only Hmong person I knew. So growing this food has been kind of like an identity project,” Judy says. “Farming has been a whole new experience of trying to understand where food comes from and appreciating food from our culture.”
Tilling the land, growing veggies and delivering the fruits of their labour to farmers’ markets and CSA customers is a very physical job, but this rich family history is what motivates Judy with every bucket of water she hauls, every wheelbarrow of soil she pushes and every time she crouches down to weed.

At ages 39 and 40, she and Hans are trying to listen to their bodies a bit more. “The first year on the farm, we were just so excited, and we went at it really, really hard. By the second season, we really felt it,” she says. “Now we’re learning how to take some care and to work in different positions to promote other muscle groups. And we’re always trying to stretch.”
Sometimes, they end their workday with a cupping session, an alternative therapy that uses suction to pull on the skin and stimulate blood flow to sore muscles, which can help address back injuries or chronic pain. (The technical term is myofascial decompression.)
“We still feel young, but we definitely feel that our bodies are not…the way they were,” Judy says with a laugh. “Recovery takes longer.”

The Nings start their mornings around 7 a.m. with a cup of coffee on the deck, surveying the farm and plotting out their to-do list. In addition to their on-site farm stand, they deliver weekly CSA boxes from June to October and, on Sundays, they sell their produce at the Picton Town Hall Farmers’ Market.
The Nings grow Hmong cucumbers, bok choy, mizuna, eggplants, Napa cabbage, yardlong beans, purple sticky corn, water spinach, peas, shishito peppers, okra, melons and more. “Some are from the seeds that my mom brought with her, so that I can stay connected with my family, and share that with my kids,” says Judy.

Judy goes for frequent walks with her 11-year-old son, who is on the autism spectrum. To minimize the pull of screens, the Nings require outdoor time from 4 to 6 p.m. for both their son and 14-year-old daughter, even if “they’re just poking things with sticks,” says Judy.
Because the Nings don’t pull the veggies out by the root, “I have to have a very strong squat game,” says Judy. This is a way to promote the health of the soil, she explains. “We leave the roots in the ground and cut the plants at the base, so the roots decompose and add more nutrients and biodiversity.”

The Nings raise Coturnix quails and a variety of hens: Wyandottes, Marans, Brahmas, Easter eggers and Olive eggers. “We get about one egg a day from our laying hens and quails,” says Judy. She says the chicken eggs taste richer in flavour because those hens prefer to forage for their food and have a more varied diet.

“Many people here haven’t heard of these vegetables before. So we thought it’d be a really good idea to share our culture with people who never experience other cultures,” says Judy. “Food is a great catalyst to bring understanding to the table—talking about recipes and sharing our childhoods has been really joyful.”
Next: This Ultramarathoner and Mom Is Bringing Reconciliation to the Trail-Running World
The pharmacist leaned towards the Plexiglass and rolled a pill bottle in her latex-gloved hands.
“So, you should definitely take this with food,” she said. “There’s a chance of stomach upset otherwise. I need to confirm, however—there’s no chance that you could be pregnant?”
I stared at her sharply. “I am pregnant. My doctor prescribed this to terminate the pregnancy.”
“Oh,” the pharmacist said. “It’s not for your stomach ulcers?”
No, I most certainly didn’t have stomach ulcers. After three miserable weeks of repeated ultrasounds, blood tests and unhappy consults with my doctor, it was clear that I had gestated a non-viable pregnancy. Now, I had finally obtained a prescription for misoprostol, which is one-half of the medications used to induce a medical abortion. It induces cramps to empty the uterus. (It is also prescribed, I noted icily to the pharmacist, as a vaginal suppository, so unlikely to upset the stomach.)
The other, mifepristone, is generally taken first, to block the hormones that sustain the pregnancy. Given the current American political climate, after the overturning of Roe v. Wade—including the fact that earlier this year, a Texas court brazenly overruled the FDA’s approval of mifepristone, describing it as “starving the unborn human”—this duo of medications has been in the headlines lately. But like all good Canadian feminists, my rage at American developments was edged with uncomfortable gratitude. How lucky I am to live in Canada, I told myself, where terminating a pregnancy is just a normal part of our healthcare, I thought.
Cue the unexpected pregnancy. I was 43 years old and, at that point, I had been pregnant twice, with two excellent children—now teenagers—to show for it. At 15 and 17, respectively, they represented pregnancies borne of a different epoch. I was in my 20s last time, and pregnancy, as a concept and an experience, had been uncomplicated for me. I expected this one to be the same, even as I felt surprised and a bit daunted by the prospect of having a young child again.
It’s only now, looking back, that I know how naïve this assumption was.
This time, I was told mine was a geriatric pregnancy. The risk of complications was high. Yet I expected the ultrasound at eight weeks to be routine, even so. My partner and I drove to a clinic on the outskirts of town, where very pregnant women sat in the waiting room, wincing with full bladders. When it was our turn in the darkened ultrasound room, I quickly noted the mood growing grim. The young ultrasound pushed her screen away from my view. Unnerved by her obviously distressed expressions and reactions, I engaged idiotic small talk. Mostly, this consisted of inadvertently pointed questions probing her discomfort. “Will we get to hear the heartbeat?” “Why isn’t the screen that I can see turned on?” “Does the doctor come to talk to everyone after they review the scans?” She wouldn’t say much.
(Related: Inside the Battle for Better Abortion Access In New Brunswick)
Soon enough, the doctor did come out. I was back in street clothes and feeling fraught. The lights were still down. My partner sat in a chair in the shadows, just a little too far away to hold my hand. The gestational sac was measuring small, the radiologist announced, and there was no heartbeat. I must have calculated the date of my last menstrual period wrong. We should go back to my family doctor and have my hCG levels monitored. Come back for another scan in two weeks.
“Is there,” I ventured, “a chance that the pregnancy might be nonviable?” Mine, as I was constantly being reminded, was a geriatric pregnancy. I had read the geriatric stats—this was not exactly unforeseeable.
“I didn’t say that,” he snapped. I should keep a positive attitude, he advised.
As we left the examination room, the tech cryptically remarked, “I’m sorry I can’t say more.”
“What does that mean?” I asked my partner in the car, as a rainstorm sent wet rivulets down the windshield. “That she saw something she couldn’t say, but that the doctor confirmed? Or that she knows something the doctor doesn’t?”
I called the walk-in clinic we’ve been using as our family doctor about the need for more testing. (I was still waiting for a referral to my OB-GYN to go through.) Like the radiologist, the walk-in doctor was upbeat. This didn’t mean anything, necessarily, he said. Plenty of pregnancies start this way and end with a healthy baby. But he never asked a basic question: how much I wanted to be pregnant in the first place.
My children were not young anymore, and my partner’s son was 15. It would be, as other women my age put it, “quite the lifestyle change.” But the rest of the world preferred only to offer their congratulations. For all the doctors and nurses and ultrasound techs I encountered, it was inconceivable that someone like me, who had spent most of her adult life as a single-parent caregiver, might feel ambivalent about being tethered to a small human again. And no one ever asked me how I was doing.
I learned that unless you are marching off to the abortion clinic, the medical system assumes you are ardently pro-pregnancy.
For the next two weeks, I had my blood drawn every other day to monitor whether my hCG levels were rising, falling or plateauing. And every other other day, I got test results. My phone would ring with my doctor’s number flashing across the screen, and I would scurry to an empty boardroom at work, close the door, and stare out the window onto a bleak, late-winter Edmonton streetscape as I braced myself. And yet, the message was still—over and over again—that I should just keep waiting. This isn’t totally out of the norm, they would say. It might still turn out okay.
For the follow-up ultrasound, we went to a different clinic. The tech working this time was in her 50s. This was a relief. I assumed that she was inured to all potential horrors of her profession.
“Just so you know,” I announced pre-emptively, “we’re not expecting good news.” I talked openly about wanting certainty more than a positive outcome. I was okay with it, I claimed, with forced sunniness. But inside, I resented that I felt more responsible for the tech’s reactions and emotions than my own.
She nodded, but as the scan progressed, her face saddened. The clinic radiologist also came to chat, as we expected, and let us know that they still couldn’t detect a heartbeat.
“Okay,” I said. “I know this isn’t exactly your area of expertise, but can I conclude this pregnancy is not viable? If so, I would like to ask my doctor for a termination.”
He hesitated. It wasn’t his area, it was true. But this radiologist also insisted that I be hopeful. It hadn’t quite been two weeks since the last ultrasound. We shouldn’t have come in so early, he said.
At the next appointment with my family doctor, I asked, point-blank, for a medical termination.
“Ah,” he said, squeamishly. “I’m not sure I’m allowed to do that.”
“But abortion is legal. Why wouldn’t this be permitted?”
“I’ll have to consult my colleagues. I’ll get back to you.”
Spoiler: He did not get back to me.
So, I remained pregnant. My hCG levels had plateaued, but they weren’t falling either. I learned later that medically, this was a “silent miscarriage,” where the fetus is no longer viable but the body continues to produce hormones to sustain the pregnancy. Unmanaged, this can put women at risk for haemorrhage and infection that can lead to sepsis or death.
Faced with the loss of a pregnancy I wanted—however ambivalently—and frustrated by the lack of clarity from my healthcare providers, I stopped being so careful about little things. I ate runny egg yolks. I went for runs and ran until I was breathless. I was empty. I was not empty. In fact, I was still 15 pounds above my normal weight. None of my clothes fit—save for, cruelly, one pair of maternity jeans that I wore to work every day.
After waiting for what felt like ages, I got my long-awaited OB-GYN consult. I love my OB-GYN (and can never understand why it’s so hard to see her), so I was relieved to finally tell her my tale. “Listen,” I confessed. “I’m okay with a 93 percent chance this isn’t going to work out. I don’t need complete certainty. I just want it to be over.”
Unlike the other doctors, she laughed.
“Oh no,” she trilled cheerfully. “This is absolutely not viable. It’s zero percent. Zero. Don’t feel bad.” I trusted her and felt immediate relief from her certainty and pragmatic reaction.
But I also felt bad for women whose pregnancies were being overseen by the other doctors I had left behind—who would never get this kind of support. In fact, I felt scared that they might not receive the care they needed.
My wonderful OB told me that I had three options: I could simply wait; we could terminate medically (with my hormone levels plateaued, just misoprostol would be necessary); or we could schedule a dilation and curettage (which is a day surgery). Waiting could take weeks, she said. It carried an increased risk of haemorrhaging and infection when I finally did miscarry. (None of the doctors touting prolonged hopefulness had mentioned this.) I could also have the surgery, but that involved general anaesthetic. She thought misoprostol would be easiest and safest. I would be supervised by the Early Pregnancy Assessment Program at the Lois Hole Hospital for Women in Edmonton, which supports women going through pregnancy loss. I was to take the pills at home, but they would call me periodically to ensure I was safe.
So, the next day, I paid for the medication. It was surprisingly cheap. I did wonder, as I left the pharmacy, why I would be mistaken for a person with ulcers. But overall, it was an unpleasant but not insurmountable weekend.
Still, all the nurses who gently oversaw my use of misoprostol assumed it was a planned pregnancy. The grief counsellor I was assigned through the pregnancy loss clinic did, too—absolutely every last person assumed a particular pro-life, ready-and-willing-to-have-this-baby trajectory. There was no space for my own terrors — about a life spent caregiving, about the heightened risks of birth defects as an older mom, which could mean carrying a child who would ask even more of me than my previous children had. By the end of the ordeal, the attitudes and assumptions felt less suffocating, but still utterly oblivious.
Later, a friend desperate for children told me about miscarrying donor-egg twins in an emergency room. She was in awe that I had had the privilege of a grief counsellor to listen to me cry and to suggest avenues of mourning she would have appreciated, but that I had felt were inane or misplaced, like naming “the baby.” My friend had had no such support, while her loss, to me, seemed much larger and vital. This was additionally confounding and distressing. The common thread, for both of us, is that we were not offered the support we needed.
My grief was complicated. I felt so very sad, but I also felt that I had been betrayed by a perinatal system intent on treating all women as if we had all chosen pregnancy and were, surely, enthusiastic child-bearers. A specialist doctor shouldn’t have had to swoop in in order for me to feel seen. All care providers should be willing to set their personal ethics aside and prioritize the mother’s mental and physical health.
The lack of recognition for me and my feelings about the pregnancy made me feel lesser-than, or like a vessel and nothing more. But it also meant I had been temporarily pushed into a higher-stakes terrain of risky medical complications, where I could have suffered even more—and dangerously so.
Next: The True Cost of an Abortion in Canada, According to an Expert
It’s a glorious, sunny morning in Los Angeles, but I wouldn’t know. I’m hiding from the world, because my eyes are swollen shut, and sore red bumps are covering the top half of my face.
I’ve been sporting this new look for two days now. I assumed it was an exaggerated version of an allergic reaction, but antihistamines didn’t alleviate it. So I reach out to my Toronto-based dermatologist who gives me an unexpected diagnosis: It’s inflammation from a moisturizer, due to the humidity in the California air. She recommends I strip back my beauty products to the bare essentials and use only a cleanser and SPF—and my skin clears within a few days.
The experience makes me question my skin-care choices. I do heaps of research when I consider buying a new product—how could I choose the wrong one? Are my other products causing harm, too? Do I really need as many products as I’m using?
A lot of people will add products to their routine that are unnecessary, and without knowing how certain ingredients will interact with their skin, says Martie Gidon, MD and dermatologist at Gidon Aesthetics & MediSpa in Toronto.
Here, Gidon shares how to build a safe, effective and minimal beauty routine.
Stick With High-Quality Essentials
Those 12-step beauty regimens? Not necessary. Gidon says the essential products for skin are a cleanser, moisturiser, sunscreen, antioxidant serum, exfoliant and anti-aging product such as a retinol or glycolic acid. “Different skin types need variations on these products since they are not all the same and the quality of the ingredients varies greatly,” she adds.
Play It Cool
Some products should be used only once or a couple of times a week. It’s tempting to use them more frequently, but that won’t speed up results—instead, it can cause irritation. According to Gidon, the ideal morning beauty routine includes a cleanser, antioxidant serum, moisturizer (if you have dry skin), and sunscreen. In the evening, just cleanser and moisturizer. One to two times a week you can exfoliate, and two nights a week you can apply an anti-aging product, which you can gradually increase frequency when your skin is able to tolerate it.
Read Your Skin
When you try a new product be on the lookout for signs of inflammation—like swollen eyes, dryness, and a rash. “Give your skin a rest from products that could be causing the inflammation,” says Gidon. “Heat and humidity, stress, and too much exfoliation could cause inflammation that would not occur in cooler weather and a no-stress situation.” If you catch the inflammation too late, it could take weeks to clear.
Changing Climates Might Mean a Change to Your Routine
“Cold weather dries skin; warm humid weather helps skin stay moister,” says Gidon. The lesson I learned: If you’re using a heavy moisturizer in a cold or dry climate (like Toronto), you may need to swap it for a lighter option in a hotter or wetter climate (like Los Angeles).
Don’t Be Wooed
Many products have acquired cult followings, but that doesn’t mean they work for everyone’s skin type. Gidon advises against the trial-and-error method of choosing products, especially when it comes to building your skin-care line-up. “Using the incorrect mix of products could be too irritating or they could inactivate each other,” she says. To make sure you’re using the best products for your skin type and using them correctly (for instance, not layering ingredients that shouldn’t be mixed), Gidon suggests seeking expert advice. “A cosmetic dermatologist can analyze skin to determine which products are best for an individual,” she says.
Next: Do You Use a Lash or Brow Serum? Beware of These Side Effects
Ciba, or sticky rice cake, is Sichuan’s version of the brown sugar mochi that is ubiquitous in so many Asian food cultures. This is usually made from heavily pounding steamed sticky rice until it forms a cake, but as my lazy self has found, it can also be made with glutinous rice flour and a microwave. This version is rolled in kinako, roasted soybean powder that you can find in Japanese and Korean grocery stores, but if you’d like, you can deep-fry the rice cakes for added texture and flavour.
Brown Sugar Mochi
Serves 4
Ingredients
- 1 cup glutinous rice flour, plus more for dusting
- 1 Tbsp granulated sugar
- ¾ cup plus 6 Tbsp of water
- 6 Tbsp dark brown sugar
- 2 Tbsp kinako
Directions
1. In a large microwave-safe bowl, add the flour, sugar, and 3⁄4 cup of the water. Whisk well to combine. Cover with plastic wrap and microwave on high heat for 2 minutes. Remove the bowl from the microwave and, using a spatula, mix the batter and pound it for about 5 minutes to remove any clumps, until the batter is smooth, solid and stretchy. Cover and set aside.
2. In a small pan over medium heat, combine the brown sugar with the remaining 6 Tbsp of water. Stir until the sugar has completely dissolved, then pour into a small bowl and set aside.
3. Place the kinako in a small bowl.
4. Generously dust a flat work surface with flour, then place the mochi batter on it and massage it to form a long log. Using a knife, cut the log into 1-inch pieces and, using your hands, form the pieces into balls. Roll and coat each piece in the kinako and place in a serving bowl.
5. When ready to serve, drizzle the brown sugar syrup on top of the mochi.
Excerpted from The Book of Sichuan Chili Crisp by Jing Gao. Copyright © 2023 Jing Gao. Photography by Yudi Ela Echevarria and Robert Nilsson. Published by Penguin, an imprint of Penguin Canada, a division of Penguin Random House Canada Limited. Reproduced by arrangement with the Publisher. All rights reserved.
Next: How to Make Vegan Desserts—The Basics of Plant-Based Baking
“Listen up cause I’ve been told, D.A.’s going after gold! We’ve been down but always rise, D.A.’s gonna get first prize!”
The members of the Dragons Abreast dragon boat team end their chant with a resounding cheer. They turn to watch a race in progress while they wait for their own heat to be called. Five long boats—each carrying 20 paddlers, one steersperson at the back and a drummer at the front—surge toward the buoys that mark the finish line in perfect synchronicity.
All eyes are on the dragonheads at the front of the boats as each team pours every ounce of their strength into pulling ahead, inch by inch. It’s still early morning and the July humidity is climbing alongside the anticipation at the Hamilton Waterfest Dragon Boat Festival.
For some of the paddlers, this is their first regatta. Others are veterans with over two decades of dragon boating and paddling experience.
(Related: As a Cancer Journey Coach and Breast Cancer Survivor, I’m Changing the Narrative for Cancer)

The History of Dragon Boat Racing
Dragon boat racing began as part of a cultural community event more than 2,000 years ago in China. On the fifth day of the fifth month of the lunar calendar (usually in late May or early June), races would be held in Chinese fishing villages to commemorate venerated statesman and poet Qu Yuan, who drowned in the river. The traditional holiday is also a time to perform rituals for good fortune and prosperity, and to ward off evil spirits. Over time, dragon boat racing evolved into what it is today: a global sport that draws in millions of athletes and spectators every year.
Dragons Abreast
The Toronto-based Dragons Abreast team stands out at this regatta for a few reasons. For one, its 79-member roster includes paddlers that range in age from 30 to 93. Prior to joining Dragons Abreast, some members hadn’t been part of a sports team since childhood and wouldn’t have described themselves as athletic. And what has brought these women together is something that none of them expected—living with breast cancer.
Breast Cancer in Canada
Breast cancer is the second most common cancer in Canada, with one in eight women diagnosed in their lifetime. Most breast cancer patients will have had either a lumpectomy to remove the tumour or a mastectomy to remove the entire breast. If the cancer has spread, they may also undergo an axillary lymph node dissection, where the lymph nodes near the armpits are removed.
Up until a few decades ago, people living with breast cancer were told to avoid physical activity. They were discouraged to take part in strenuous and repetitive upper body movement, because it was thought that exercise could cause lymphedema. This chronic condition, which has no cure, is characterized by swelling of the arms and hands caused by lymph fluid that can’t drain due to the surgical removal of lymph nodes, or damage by radiation.

Dragon Boating for Breast Cancer Survivors
In 1996, Don McKenzie, a sports medicine physician and professor in the faculty of kinesiology at the University of British Columbia, launched a study to challenge the exercise-lymphedema connection. He recruited 24 volunteers, all with a history of breast cancer, to participate in a six-month-long dragon boat program. With its focus on paddling—which requires intense, repetitive upper body movement—the sport was the perfect vehicle to test out his hypothesis: that exercise didn’t cause lymphedema and would, in fact, be beneficial to survivors.
At the time, it was a bold experiment filled with unknown risks—and it paid off. There were no new cases of lymphedema among the women, several of whom reported improved range of motion in their shoulders and better mental health. The group made its debut as Abreast in a Boat at Vancouver’s 1996 dragon boat festival, officially becoming the world’s first breast cancer survivor dragon boat team.
McKenzie’s study was hugely influential in setting a new course for breast cancer recovery. Since then, there have been several more studies recognizing that exercise doesn’t cause lymphedema, and that it can actually reduce the amount of lymphedema that patients experience over time. Further research has shown that dragon boating offers survivors improved heart function, the benefits of community and improved health-related quality of life.
The breast cancer survivors on this team are in the same boat, literally and figuratively. For many, being part of a community that knows intimately how life changes after breast cancer is as beneficial as the physical gains. The team offers a supportive space to navigate all the complexities of survivorship, from regaining confidence post-treatment to remembering those who’ve passed on with a flower ceremony.
“I was so surprised at how emotional racing was for me,” says Liz Johnston Hill, the race coordinator for Dragons Abreast. “It’s almost overwhelming how people encourage you, no matter what.”
Today, there are more than 310 teams from 37 countries that are part of the International Breast Cancer Paddlers’ Commission—and 50 of them are from Canada.
When Dragons Abreast founder Eleanor Nielsen, now 85, was diagnosed in 1989 with stage two breast cancer, she underwent chemotherapy and a mastectomy, and had her lymph nodes removed. Back then, her doctors advised her to avoid using her surgical side.
“I was told I shouldn’t vacuum and carry groceries,” she recalls. “There was a whole pile of things I shouldn’t do.”
While working at the Canadian Cancer Society to help grow and promote their programs, Nielsen attended a conference in Vancouver, where she met members from the original Abreast in a Boat team.
“When I came home, I asked my husband, ‘Should I start a team in Toronto?’”

Dragon Boat Racing in Toronto
That led to the formation of Dragons Abreast in 1997. Now in its 26th season, the team has welcomed over 300 women and men living with breast cancer onto the boat. Together, they’ve travelled the world to compete in places like Panama, Australia and Italy.
In celebration of the team’s 25th anniversary last year, they paddled through Ontario’s Trent-Severn Waterway. Over six days they raised $38,000 for the Breast Cancer Support Fund, a nonprofit providing financial assistance to patients in need.
In 2021, Nielsen co-authored Internationally Abreast: Exercise as Medicine, which documents the history and rise of breast cancer dragon boat paddling across the world. She summarizes why the sport is integral to many survivors with a quote from McKenzie: You aren’t racing against each other; you’re racing cancer.

Regatta Day
Today at the regatta, Dragons Abreast members rest up at their tent. Lounging in camping chairs, the women chat and joke, passing around snacks like homemade baked goods, frozen orange slices and pretzel twists.
Pink is everywhere: the fuchsia Dragons Abreast logo, the light pink breast cancer awareness ribbons, hot pink tutus and manicures, and one member’s glittering sequin baseball cap adorned with pins collected from international regattas. It’s not hard to spot a breast cancer team, but the signs of cancer are sneakier.
Akaash Singh’s Journey With Breast Cancer
For Akaash Singh, 55, it was dryness around her nipple. Her first mammogram was clear, and Singh, who works in the pharmaceutical industry, just continued on with her demanding career.
“I saw the changes, but they were so gradual,” she says. “We know to look for lumps, but we don’t necessarily look for skin changes or associate that with cancer.”
Within a year, the symptoms progressed to redness around the areola and an inverted nipple. And they weren’t going away. Singh went back to her doctor and was immediately recommended to a surgeon, who felt a lump in her milk duct.
The biopsy came back positive for cancerous growth. Following Singh’s localized stage three diagnosis in 2012, she underwent a full mastectomy with lymph node dissection the day before her 45th birthday.
Singh joined Dragons Abreast after she finished treatment in 2014, and is now the organization’s chair. Before her diagnosis, she considered exercise to be secondary to work.
“I never really took that time for myself to keep my body healthy,” she says. Dragon boating has helped Singh reprioritize her health. “I’m not a morning person, yet I would get up at five if I had a regatta that day,” she says. “Something I wouldn’t do for anything else in my life.”

Benefits of Exercise and Breast Cancer
As the medical director of the After Cancer Treatment Transition clinic at Women’s College Hospital in Toronto, Carol Townsley stresses the importance of physical activity with all of her patients. It’s now standard to integrate physical activity into a recovery plan, all the way from light stretching to more rigorous sports like dragon boat, depending on the patient’s baseline fitness and comfort level.
“Breast cancer survivors are on drugs like tamoxifen or letrozole, which are estrogen blockers, and these drugs can have a lot of muscle or joint side effects,” she says. “There’s a lot of evidence that being active minimizes the side effects of these medications so [patients] can stay on them longer, which, in turn, decreases their chance of recurrence.”
From Townsley’s experience, patients who participate in group sports like dragon boating have better outcomes because of their camaraderie and dedication.
“One of the things that I’ve found as a clinician is that the passion patients have for dragon boating is unique,” she says. “If we can look for anything in sports or exercise, sticking with it and enjoying it is key.”
Shelagh Tyreman’s Experience With Breast Cancer
Shelagh Tyreman’s soprano voice rang sharp and clear as she sang the national anthem at the regatta. When the music stopped, her Dragons Abreast teammates burst into applause—a familiar sound to the 60-year-old classical musician. She began her training as a pianist, later switching to opera singing.
After performing all over the world, from Notre Dame to the Vatican, Tyreman is now a teacher and the music director for St. Andrew’s Presbyterian Church in Brampton. She was diagnosed with breast cancer in 2012 and completed treatment that same year, after a lumpectomy, six months of chemotherapy and six weeks of radiation.
But in 2019, she had a gut feeling that something was off. After having multiple clear mammograms and ultrasounds over the next three years, Tyreman finally confirmed her fears: a recurrence. Although she’s in active treatment again, dragon boat practice is still part of Tyreman’s weekly routine.
“Every time I have an appointment, the doctors tell me, ‘Whatever you do, keep paddling because it just keeps you so strong and fit.’”

Somebody to Lean On
When Tyreman was first diagnosed in 2012, she kept her condition private and didn’t meet with any support groups. ”I just couldn’t at that time,” she says. “I felt very private about my diagnosis.”
Now, she credits Dragons Abreast and dragon boating for helping her face the second round. “I felt so betrayed by my body because I did everything I was supposed to and you just want to move on with your life,” she says.
“Paddling has given me not only physical strength but mental belief in the power of myself, of my soul, of who I am.”
Even when Tyreman feels nauseated from taking her oral chemotherapy drugs, being out on the water and with her teammates has become a healing balm.
“I know that if I’m having a rough day because of something to do with breast cancer, there’s about 40 to 60 people I can talk to,” she says. “I’m not alone anymore.”
Angela Fong, an assistant professor at the School of Kinesiology at the University of Michigan and the Rogel Cancer Center, agrees that dragon boating is a valuable way for patients to bond. Things like after-practice socials, spending time to master techniques and the competitive nature of racing all contribute to helping people move on from their diagnosis.
“They see themselves as survivors, but they also see themselves as athletes,” she says. “This additional social time allows them to talk and process that whole experience.”

Finding Support as Survivors Through Dragon Boating
Tyreman stepped into a dragon boat for the first time seven years after her initial diagnosis. In 2019, she saw on Facebook that Dragons Abreast was having an open house to recruit new members and jumped at the chance.
“I was finally ready to do something publicly about being a breast cancer survivor,” says Tyreman. Although she had never paddled before, Tyreman knew that she wanted to seek out the community. “I was looking at all these strong breast cancer survivors,” she says. “I thought, I’m ready to meet them and maybe be one of them.”
After a long day of dragon boat racing, the members of Dragons Abreast proudly sport tangles of gold medals and bright pink ribbons around their necks as they pose triumphantly for a group photo.
In dragon boat racing, the difference between winning and losing can come down to less than a tenth of a second. For the team that day, it was a win by 0.13 seconds. But the paddlers insist they had already won before they ever stepped into the boat.
“You learn so much from all of these incredible women,” says Singh. “That not only makes you a better dragon boater, it also makes you a stronger person, and more comfortable in your skin.”
Next: Jeanne Beker on Finding Community and Support Through Her Breast Cancer Diagnosis