8 Reasons to Request an Earlier Mammogram
Experts recommend you start mammograms at 45 or 50; however, there are some factors that may make you want to start breast cancer screening earlier.
According to Health Canada, “women who are 50 to 74 years of age should have screening mammograms every two to three years.” The American Cancer Society suggests women of normal risk begin annual mammography at 45. Meanwhile, women as young as 20 can get breast cancer. As a result, there’s a bit of a gray area when it comes to what doctors recommend for their patients. “The underlying evidence supporting the use of screening mammography stems from nine randomized trials that began between 1963-1991 in the United States, Sweden, the United Kingdom, and Canada and studied women at average risk for breast cancer,” explains Kristi Funk, MD, FACS, breast cancer surgeon and medical director at Pink Lotus Breast Center. “However, that data is now decades old and new advances in the field of breast cancer detection and treatment have caused experts to question whether or not the guidelines deserve a makeover.” Here’s a look at some of the reasons why you might want to consider requesting yearly mammograms well before the age of 50.
You have a personal history of breast cancer
Even if you didn’t have full-blown breast cancer, but a high-risk lesion was found via biopsy from your breast, you should be getting mammograms earlier than the recommended age of 45 for average-risk women. “Specifically, women who have had a breast biopsy that shows precancerous cells (specifically, atypia or LCIS) should request an earlier mammogram,” says Dr. Funk. (Check out these breast cancer advancements that can help the fight against the disease.)
You have a family history of breast cancer
A woman’s risk of breast cancer nearly doubles if she has a first-degree female relative who has been diagnosed with breast cancer. First degree means your mother, sister, or daughter. If two of those first-degree relatives have been diagnosed with breast cancer, your risk rises to 60 percent, or five times higher than average. Researchers also know that your risk also goes up if a brother or father has been diagnosed, although they are not sure the exact increase in risk posed by this circumstance. Add these foods to your plate to help lower your risk of breast cancer.
You know of genetic mutations in your family
There are many gene mutations that have a link to cancer, but the most common for breast cancer are BRCA1 and BRCA2. “On average, women with a BRCA1 mutation have up to a 72 percent lifetime risk of developing breast cancer and 69 percent risk for women with a BRCA2 mutation,” says Nancy Elliott of Montclair Breast Center. “Breast cancer that is positive for the BRCA1 or BRCA2 mutations tends to develop more often in younger women.” Experts recommend that anyone with these mutations be monitored carefully and discuss risk with a doctor who specializes in breast cancer.
You were exposed to radiation therapy between ages 10 and 30
Research published in the Journal of the National Comprehensive Cancer Network has linked exposure to ionizing radiation as one of the key risk factors for the development of breast cancer. Much of the data come from the study of atomic bomb survivors as well as women who were exposed to medical radiation for either diagnostic or therapeutic purposes. If you were exposed to radiation for any reason during the ages 10 to 30, discuss it with your doctor to determine the ideal age to start mammograms.
There’s a history of cancer in your family
The lifetime risk of developing cancer over the course of your life is about 1 in 3, which explains why most people have a family member or friend who’s been diagnosed with cancer. But if there happens to be a great deal of cancer in your family—what seems like more than usual—it’s worth mentioning it to your doctor to see if you qualify for an earlier mammogram. “Particularly, if you have two or more family members on the same side with breast, ovarian, pancreatic, prostate, melanoma, uterine, colon, and/or stomach cancers, you should request an earlier mammogram,” says Dr. Funk.
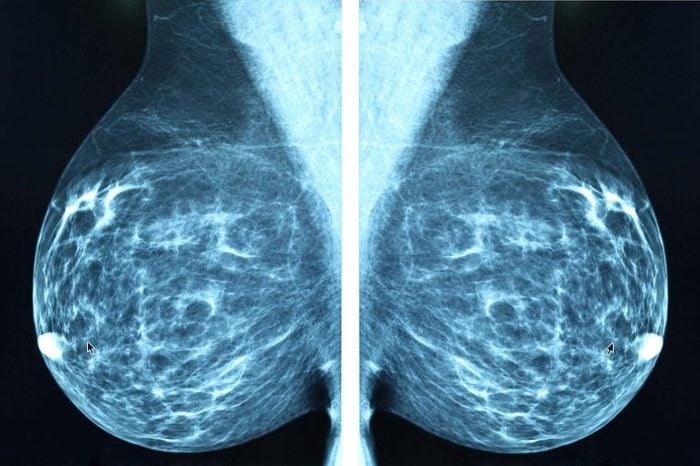
You have dense breasts
Dense breast tissue is quite common, and researchers have unfortunately linked it to an increased risk of larger tumors or more advanced cancer at diagnosis. Dense breast tissue can make it more difficult to detect problems on a mammogram, which is why women at high risk and/or with dense breasts may benefit from a more sensitive test: breast MRI. “Unfortunately, we’ve seen women skip their MRI and then get diagnosed down the road,” says Dr. Elliott. “We always wonder if it could have been caught earlier and if they could have avoided chemotherapy.”
You notice a lump that doesn’t go away
It’s not uncommon for women—especially young women who are still experiencing a monthly menstrual cycle—to notice a lump in the breast. This is even more likely if you are breastfeeding, as the breast tissue is constantly changing due to milk production. Most of the time there is nothing to worry about and the lump goes away on its own. However, if you notice a palpable breast lump that doesn’t go away with your menstrual cycle (if you still have cycles), Tara Shirazian, MD, a gynecologist at NYU Langone Health, recommends requesting a mammogram.
You experience nipple discharge or changes on the skin
Nipple discharge is common in women with breast cancer. In fact, it is the third most common symptom after breast pain and the presence of a lump, according to research published in Radiologia Brasileira. If you notice nipple discharge that is persistent and especially if it is one-sided, schedule an appointment with your primary care physician or gynecologist who may recommend that you schedule an earlier mammogram.
How can you find out your risk?
One in eight (12 percent) women will be diagnosed with breast cancer during their lifetime, according to Health Canada. To determine whether you’re at average or increased risk, Health Canada recommends having regular screening tests. The American Society of Breast Surgeons (ASBrS) recommends undergoing formal risk assessment for breast cancer between ages 25-30 and the American College of Radiology (ACR) and Society of Breast Imaging (SBI) advise all women to undergo risk assessment at age 30, explains Dr. Elliot. “These results help women and their physicians determine when they should start screening—and what type of screening they’ll need,” she says. “High-risk women may need to be screened earlier and should consider supplementary screening, such as ultrasound or MRI (in addition to annual 3D mammography).”
Next, learn how one weekend completely changed her life after breast cancer.




