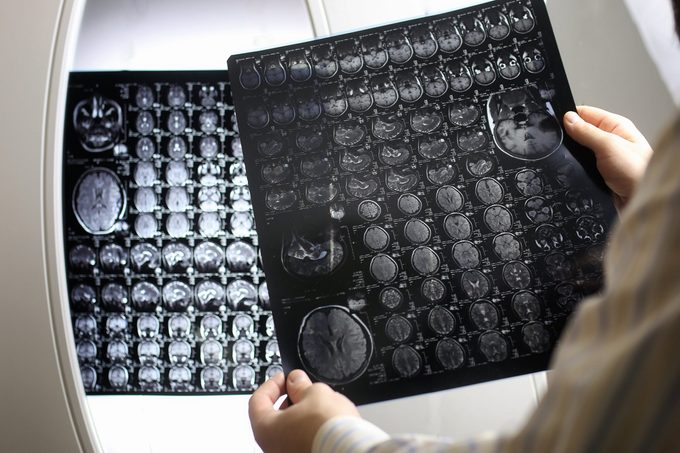
This Is What Your Brain Looks Like with PTSD
On brain scans, people with PTSD have distinct differences compared to people without it—but not every PTSD brain is the same.
Post-traumatic stress disorder, or PTSD, is distressingly common: The Canadian Mental Health Association notes that only eight percent of people will experience this condition in their lifetime.
PTSD is a “trauma and stress-related disorder with links to anxiety and dissociative disorders,” explains Julia Breur, PhD, a licensed clinical psychotherapist in Boca Raton, Florida. It’s caused by exposure to a traumatic event. People with PTSD may have recurring dreams or flashbacks of the event and extreme psychological distress. Exposure to actual death or threatened death, sexual violation, or serious injury are some of the triggers associated with PTSD, which Dr. Breur adds are also outlined in the American Psychiatric Association’s (APA) fifth edition of the Diagnostic and Statistical Manual of Mental Health Disorders (DSM-5).
“The disturbance, regardless of its trigger, causes clinically significant distress or impairment in the individual’s social interactions, capacity to work, or other important areas of functioning,” says Breur.
Clearly, PTSD takes a toll on your brain; the distress and associated responses play a role in what your brain looks like with PTSD. Here’s what’s happening: “Our brains are built in a way that we remember or forget memories depending on their importance to our survival, how recently they occurred, and what happens immediately before or after the event,” says Israel Liberzon, MD, a professor and head of the Department of Psychiatry at the Texas A&M College of Medicine. He explains that any dysregulations that may develop in the PTSD brain are often dependent on what people bring to the trauma in the first place, as well as the severity of the experience and how they cope with the experience post-trauma.
Brain regions affected by PTSD
There are some common brain regions that are most commonly impacted by PTSD. Melanie Greenberg, PhD, a clinical psychologist in Mill Valley, CA and author of The Stress-Proof Brain, says that the amygdala acts as the brain’s threat-detection center and is responsible for responding to a threat or danger. The hippocampus is another region implicated, which is associated with storing memories in an organized way. The prefrontal cortex—more specifically, the medial prefrontal cortex—is yet another region often altered by PTSD; its role, Breur explains, is to “modulate emotional responsiveness.”
The amygdala grows
So, what exactly does your brain look like with PTSD? Greenberg explains that if you have PTSD, you may overreact to threats. This is where the amygdala enters the picture. “The amygdala is the brain’s threat detection center,” she adds. It’s in this fight-or-flight brain region where it’s not unusual for a PTSD brain to show an increase in volume, says Greenberg. If you’re feeling like you’re in “fight” mode more often than not, here are some reasons why you might be more stressed than you realize.
The hippocampus shrinks
The hippocampus is the brain’s center for verbal memory and is where you store memories, Greenberg says. With PTSD, in some cases it will decrease in size, she notes. The result may be that memories may surface but often only in fragments; for example, if you were sexually abused, you may sometimes see a related image, but the memory isn’t fully formed. Therefore, you can’t understand the memory or experience in its entirety. Interestingly, a study published in 2018 in PLOS ONE reports that “the right hippocampus seems to be more strongly associated with PTSD than the left.”
The prefrontal cortex contracts
This area of the brain can calm the amygdala, says Greenberg, but it can lose volume in people with PTSD. That can result in interference with judgment and decision making.
Each PTSD brain varies
While these are the main brain regions that Dr. Liberzon says tend to be implicated in a “vast majority of PTSD individuals,” he notes that each PTSD individual can have brain variations. In other words, there isn’t a one-size-fits-all image for everyone with the condition. He says that for each person, there are different combinations regarding the deficiencies in each brain area.
Therapies to help manage PTSD
“A PTSD brain can improve,” Breur states. “The hippocampus can begin regulating memories again, the amygdala can calm down, and the medial prefrontal cortex can revert from reactive to restorative mode.” Cognitive behavioural therapy (CBT), she says, is one kind of treatment that’s been “proven to increase hippocampus volume in PTSD sufferers.”
Additionally, mindfulness may help. Greenberg writes in her Psychology Today blog, The Mindful Self-Express, that mindfulness interventions “lasting ten to 12 weeks have been shown to decrease amygdala volume and increase the connectivity between the amygdala and PFC. Mindfulness seems to make the amygdala less reactive and the PFC more able to calm down the threat response.” Here are four simple ways to practice mindfulness even on the busiest of mornings.
Eye Movement Desensitization and Reprocessing therapy (EMDR) may also help with PTSD. The American Psychological Association explains that it works by using eye movements in conjunction with rhythmic left-right stimulation such as tones or taps. “While clients briefly focus on the trauma memory and simultaneously experience bilateral stimulation (BLS), the vividness and emotion of the memory are reduced.” Medication can also be beneficial; the Mayo Clinic notes that antidepressants and anti-anxiety medications may manage PTSD symptoms.
Can ecstasy help manage PTSD?
Interestingly, there is even some research indicating that MDMA, also known as ecstasy, can decrease PTSD symptoms when used together with psychotherapy treatment. Information published in a 2019 issue of Psychopharmacology states that studies conducted by experts at the University of British Columbia Okanagan campus have found “…significant symptom reductions in a large sample of participants with PTSD treated with active doses of MDMA combined with psychotherapy.” More studies need to be done before the FDA can approve it, though some sources suggest that could be as soon as 2021.
Next, find out which diseases strike women more than men.




