What is Body Dysmorphia? 5 Signs You Have Body Dysmorphic Disorder
Body dysmorphia is an obsession with a perceived flaw on your face or body. Experts share the signs and how to seek treatment.
When Los Angeles bodybuilder and fitness coach Lindsey Marie Greeley was just 17 years old, she competed in her first bodybuilding show. She would stare in the mirror in the weeks leading up to competitions, “trapped in her head,” obsessed with having the perfect body. She would be devastated by a third-place ranking and by “constructive criticism” from the judges such as “You still aren’t small enough; you need to lose more weight.”
Before long, she’d developed body dysmorphic disorder (BDD), along with an eating disorder. The condition strikes over 350 000 Canadians, and not just athletes and bodybuilders.
(Related: Do You Have a Healthy Body Image?)
BDD diagnostic criteria
Some people don’t like part (or all) of their body, but BDD goes beyond dissatisfaction. According to the psychiatric manual DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition), this is the criteria used to indicate a patient has BDD:
-
Preoccupation with nonexistent or slight defects and flaws in appearance
-
Repetitive or compulsive behaviours, such as mirror checking or changing clothes many times
-
Clinical significance, meaning the obsession must cause significant distress or must inhibit everyday functioning, such as a person’s social life
-
Differentiation from an eating disorder, which ensures that the clinician shouldn’t actually be diagnosing the person with an eating disorder
-
There are two additional further distinctions to the diagnosis:
-
Muscle dysmorphia: A person is particularly worried about their body build (muscles) being too small or insufficient. This specific type has been linked to higher suicide rates and poorer quality of life than other types.
-
Insight specifier: How accurate or inaccurate a patient’s perception of themself is.
-
Beth Rosenbaum is a Philadelphia-based licensed clinical social worker and therapist with over 30 years working with eating disorders and BDD. She says that there can either be an infatuation with reaching a certain size or weight, or people can have a preoccupation with how a certain body part looks. She typically sees women obsessing over their breasts, stomachs, and thighs, trying to fit the “societal perfection expectations for women.”
For men, often it’s the stomach, chest and muscles, abs, biceps, and a concern they aren’t meeting a standard as well. She’s also careful to differentiate between BDD and body dissatisfaction, which many Canadians struggle with.
The emotional toll can be severe, with people thinking about the body part(s) they hate many times per hour, disrupting their daily lives and ability to concentrate.
(Related: These Proven Ways Can Help Boost Your Body Image)
What causes BDD?
There isn’t one cause, but a variety of triggers in conjunction with past or current traumas in the patient’s life. Rosenbaum says it’s often a result of underlying emotional issues that need to be addressed. She also sees most people with eating disorders also suffering from BDD as well.
Societal standards, social media scrolling, and the inaccurate idea that our lives would be better if we were a smaller size, are all to blame, Rosenbaum explains. Mixed messages about society’s expectations don’t help either.
She describes women’s magazines which she says traditionally have told women in particular conflicting messages: “On one side of the cover, it’s the miracle diet next to how to bake the perfect cake. I did a research project on conflicting messages…what do we do with that?”
BDD can also be associated with transgender patients who are transitioning.
“People who were born with a female gender [and now identify as male] may have a hard time with breast development and hips and stomach, and that too can lead to eating disordered behaviour,” Rosenbaum says. She also sees other major bodily transitions, such as pregnancy and postpartum life, being a trigger for BDD. “You could lose all the ‘baby’ weight but your body proportions have changed,” she says.
(Related: On the Pursuit of Perfection—Are Our Social Media Habits Harming Our Self-Worth?)
Signs of BDD
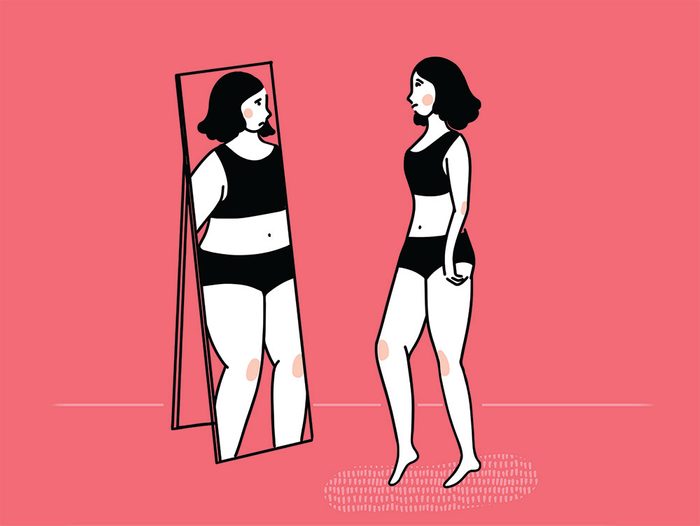
Your idea of a “flaw” isn’t realistic
The Diagnostic Manual differentiates between people who are actually obese and are worried or struggling with that, and BDD. With BDD you are concentrating on minute imperfections that are normal aspects of being human, rather than actual body issues that are visible to others.
Samantha DeCaro, an assistant clinical director at The Renfrew Center of Philadelphia, says BDD is a fixation on “perceived” flaws.
“These flaws are not detectable, or they are barely noticeable, to anyone else,” she says. “People with BDD commonly become obsessed with real or imagined imperfections on their face, their hair, or the size and shape of a particular body part.”
You avoid social situations
Ever canceled an event because you can’t find something that makes you look skinny enough to go out? This is a concerning sign that can indicate BDD. Psychotherapist Haley Neidich, a licensed social worker with an online private practice, says those with BDD may “isolate themselves and avoid social situations.”
Rosenbaum says the major distinction that helps her diagnose BDD is identifying “how much does this interfere with [a patient’s] life?” “How much of my thinking time does this take? Does my focus on my body keep me from doing things I enjoy, like going out with my friends?” All of these can indicate that you are moving from body dissatisfaction to a more concerning, obsessive disorder.
(Related: 15 Things About Social Anxiety Disorder Psychologists Wish You Knew)
You spend a lot of time staring in the mirror
When bodybuilder Greeley finally reached her lowest point and reached out to a therapist, she was diagnosed with BDD, as well as bulimia. “When you are in that world staring in the mirror taking thousands of [progression] photos for coaches, I’d say ‘I can’t see my abs, Oh God,'” she says. Greeley would spend hours “stalking” other people’s Instagram accounts, comparing her body to theirs. “I felt not skinny enough. It became sick and obsessive,” she says.
You can’t stand your own face
Rosenbaum says the pandemic has worsened BDD for many people who are sitting on Zoom calls for hours, staring at their own reflection. She jokes that even she has never “checked her hair” this much.
“People are staring at their distorted image all day. For most of us, we are bodies from the chest up. We don’t even have bodies,” Rosenbaum explains. This unreasonable amount of time we can now spend staring at our own features is exacerbating the problem. It’s being called the “Zoom Boom” as plastic surgeons see more patients considering plastic surgery in 2020. Recent research from the American Society of Plastic Surgeons reveals telemedicine calls for plastic surgery are up 64 percent.
DeCaro says we are living in a society obsessed with “fatphobia and ageism,” which causes everyone to be critical of their bodies from time to time, but those with BDD can be constantly concerned with “real or imagined imperfections on their face” or other body parts.
You see your body as parts, not a whole healthy being
Finding yourself hating a specific body part? This can be one of the difficulties of BDD, as piecing out the body causes us to hyper analyze the flaws of each part, rather than looking at the body as a whole being, Rosenbaum explains. One of the strategies she’s found helpful with patients is helping them to see their bodies as a whole being that serves a function, and to focus on what your body can do.
“Appreciate what your body does for you. Every aspect of your body. Learn to appreciate what it does and how it serves you so well… so we need to feed our bodies with fuel to give us energy so our brains work. So we can walk and love and engage in everything our bodies do. Often [people with BDD] only focus on the surface,” Rosenbaum says. That deep dive into our perspective on our bodies, and focus on the importance of certain parts being perfect, is what BDD patients work on in therapy.
(Related: Body-Positive Quotes to Remind You All Bodies Are Beautiful)
What to do if you think you have BDD
First, determine the severity of the symptoms. Often BDD happens in conjunction with an eating disorder, which can be more dangerous than BDD by itself.
Neidich says individuals with BDD are known to pursue or complete medical procedures in order to change their bodies in an effort to rid themselves of the obsession, which can be dangerous. “Given the high prevalence of disordered eating among individuals with BDD, it is important to point out that eating disorders are the most deadly mental health disorder,” she says.
Behaviours Rosenbaum says can be more severe including binging and purging, restricting calories, overexercising, and other typical eating disorder symptoms. Seeking therapy is an important step towards overcoming BDD, and is a great place to start.
Next steps
Neidich suggests the following steps, noting that BDD often occurs along with another condition (comorbidity):
-
People with co-morbid personality disorders may be referred to dialectical behaviour therapy (DBT) treatment, a type of cognitive behaviour therapy that helps teach skills to handle negative emotions.
-
Those with co-morbid post-traumatic stress disorder (PTSD) may be referred to a trauma therapist.
-
Anyone with obsessive-compulsive disorder (OCD) may be referred to a specialist for cognitive behaviour therapy (CBT) combined with Exposure and Response Prevention, a type of therapy that exposes people to their fears.
-
Those with co-morbid substance use disorders will be encouraged to attend 12-step programs and focus on sobriety.
-
Individuals with eating disorders should have a multidisciplinary treatment team.
“Just like other mental health conditions, it is possible for people to reach a place in their recovery where they are no longer symptomatic (or minimally so),” Neidich says. “However, individuals with a history of BDD are at a high risk for a recurrence of the symptoms or other mental health conditions in the future, particularly around a time of transition or intense stress in their lives,” she explains.
Greeley is finally able to manage, after years of therapy. She says you don’t just wake up and not have BDD anymore, and that sometimes she still has to check herself: “It’s OK to have one Oreo. You can have a cheeseburger and it won’t be the end of the world,” she says. She credits her care team’s support with helping her “learn to love herself all over again.”