Can You Reprogram an Injured Brain?
An expert explains how we can reprogram cells, why the gut-brain connection is so exciting and what personalized medicine means for women’s health.
Maryam Faiz’s path to neuroscience wasn’t exactly a straight one. She considered architecture. She flirted with urban planning. She took a summer off from her PhD to intern at the BBC and spent another summer in Croatia tracking dolphins across the Adriatic. But a fascination with stem cells—and a meeting in Sweden with one of Canada’s leading experts in regenerative medicine—finally drew her to the lab. “When you see a neuron, it’s almost like space—you don’t know exactly what it is, but it’s just so beautiful,” says Faiz, a professor at the University of Toronto’s Faculty of Medicine. “There’s a feeling of unmitigated possibility.”
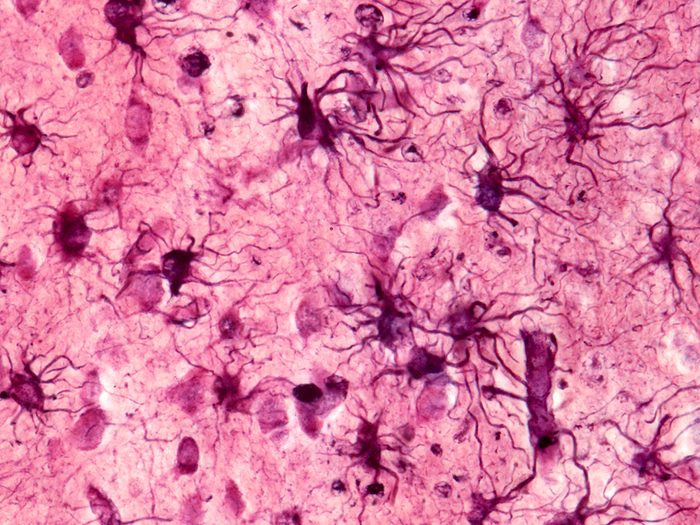
Her research now focuses on a promising class of star-shaped brain cells called astrocytes. “They’re a kind of glial cell, because glia is Greek for glue, and astrocytes were historically thought of as the sticky stuff that held the neurons of the brain together,” Faiz says. Whoops: Turns out scientists were selling astrocytes short. They actually play a huge role in the brain’s circuitry, regulating blood flow and controlling how information travels across the brain. Not only that—as Faiz and her team are learning, astrocytes may also be harnessed for brain repair, offering the future possibility of custom-made therapeutics for people suffering from neurological injuries and diseases. “Astrocytes are quite hot at the moment, in terms of things to study in neuroscience,” she says with a laugh.
(Related: The Secret to Learning a New Skill at Any Age)
What can go wrong with our brains?
Lots. Broadly speaking, the brain is not a regenerative organ, like the skin or even the liver. You don’t generally regenerate neurons—they’re kind of fixed. So you can have changes in the way the brain develops, and that can lead to neurodevelopmental disorders. You can have an injury, like a stroke, and lose neuronal cells. And then there are neurodegenerative diseases, like Alzheimer’s and Parkinson’s disease, where your neurons become under attack and start to die off.
When we lose these neurons, what impact does it have?
I can give you a personal example. My younger sister had a traumatic brain injury, and she lost neurons in a region of the brain that’s important for verbal communication. It was a small injury, and she was able to recover—because even though you lose neurons, the neurons around them can reconnect, which we broadly refer to as neuroplasticity. But my sister still has problems with speaking. The word school is problematic for her, because she can’t connect the sounds to the letters, so she’ll say shul.
The human brain is so interesting because it has this innate ability to rewire, kind of like an electrical circuit. But even small changes in neuronal loss can lead to pretty big impairments in function. And so depending on the region of the brain, you can have different types of impairments, whether that be vision or motor or cognition.
How does your work help with these sorts of impairments?
My lab studies astrocytes, which are really important for proper brain function: They fine-tune neuronal information, so they can make that information transmit further, or they can dampen it down. But after injury or disease, some types of astrocytes can become pathological and even start to kill neurons. One example was work out of Harvard on progressive multiple sclerosis—and this was preclinical, in mice, not in humans. It showed that if you just removed astrocytes in this end stage, you got improved function.
What we want to do in my lab is create new cells. Basically, you can take any mature cell and hit it with a bunch of genes that are important for its conversion to a new cell type. And so we started by reprogramming astrocytes into neurons. Again, this is preclinical—nothing to do with humans—but in mice after stroke, reprogramming improved mobility and gait to the level of an uninjured animal.
So you can transform the astrocytes that limit brain recovery into cells that are helpful instead?
I think the only way that reprogramming will work is if we’re able to generate really specific therapeutics. And that’s where it’s important to understand the role that different astrocytes play in different types of diseases at different points in that disease. Imagine a scenario where we’ve identified Astrocyte Type A15, which happens at a certain time post-stroke and is really deleterious. We could go in, target it, change it into another type of cell and leave all the other cells that are important for recovery.
Are there different factors that influence how astrocytes respond to injury or disease?
Over the last couple of years—this is so exciting—there’s been a clear link between the gut and the brain. We know that the bacteria that colonize your gut are really important in brain development, and also really important for neurodegenerative diseases and even injury. So after a stroke, for example, the bacteria in your gut gets altered. And we think this bacteria feeds back onto the brain and can affect the neuroimmune response. We have some really nice data—again, preclinical—that shows that just by using probiotics after stroke, it actually improves motor function. It’s wild. So one of the cool things we’ve started looking at is how different types of bacteria in the gut change the astrocyte response in the brain. We think that could be important for developing really novel therapeutics for brain treatment that you could administer in the gut.
It sounds like this is leading to more and more bespoke therapeutics.
That’s what our lab is all about. I think we’re in an era of personalized medicine. Especially in a system like the brain, which is so precise, you need to think about bespoke therapeutics. You’re not going to want to take out all astrocytes, which are so important, and you’re not going to want to put back all types of neurons. This allows us to be really specific.
And what are the benefits of such a specific approach?
I mean, we’re humans, right? There’s so much variation that there can never be a one-size-fits-all response. I think a lot of clinical trials and drugs have failed in that respect. Even if you just think about women’s health, 50 percent of our population was almost never tested. And so many of the drugs that have traditionally worked in men don’t work in women. Even if we could just conquer that, I think it would be amazing. But with personalized medicine, you start to make discoveries that are going to work no matter where you’re from, or what your background is, or your genetics or your sex or your age. That’s where the next 10 to 15 years are going to be really exciting.
Is that what keeps you motivated in your work?
Science tends to be quite incremental. But I do think, within 10 to 15 years, we could actually make a big difference with cellular reprogramming. And that helps us keep focused and on track to do the next experiment that’s going to take us to the next step that’s going to make the biggest difference in people’s lives.
Next: These Activities Help Prevent Dementia, According to a New Study




